Abstract
Torticollis is defined as an imbalance of the sternocleidomastoid muscle (SCM), with less extension of the neck, resulting in a preference to turn the head more from one side to the other. The characteristics frequently found are: ear contralateral to the torticollis displaced forward, facial asymmetry, and contralateral occipital flattening, as well as a smaller ipsilateral eye, causing misalignment of the eyes. This condition can also cause mandibular inclination (MI), in the frontal plane, with a difference in opening between the maxilla and mandible from one side or the other. The diagnosis and treatment of torticollis are routinely carried out by the physiotherapist and the diagnosis of this mandibular inclination is traditionally through visual examination. This assessment of mandibular inclination, carried out by the dentist, in an objective manner, can contribute to the diagnosis and also to the monitoring of proposed treatments that should reduce mandibular asymmetries. The objective of this study was to create a protocol for objective measurement of the distance between the maxilla and mandible, on the right and left sides, using photogrammetry, to detect whether mandibular inclination can be observed by the shorter inter-arch distance on the side corresponding to the torticollis. Case reports of two babies (1 baby aged 9 months and another aged 1 year and 1 month), diagnosed with congenital torticollis. Photogrammetry was carried out: the babies were positioned on a dental stretcher and photographed in maximum opening, intermediate, and closing positions. Using the photos and the IMAGE J program, measurements between the maxilla and mandible were taken (see photogrammetry description). Results: The measurement protocol used in both babies confirmed the greater mandibular inclination by approaching the hemi-arch corresponding to the side of the torticollis, compared to the opposite side. Objective measurement of mandibular inclination can be part of the timely diagnosis for congenital torticollis. Studies with an adequate sample size and methodology are necessary to confirm this diagnostic tool.
1. Introduction
Congenital torticollis is defined as a postural imbalance arising from unilateral shortening of the sternocleidomastoid muscle (SCM), evident at birth or after birth. It is characterized by having less extension on this side of the neck, due to cervical flexion, tilting the ear towards the shoulder, and also due to contralateral cervical rotation, turning the face towards the opposite shoulder [1-5].
Limitation of neck movement can be caused by being a firstborn baby (more contracted uterus and vaginal structures), twin pregnancy, intrauterine position (restricted in the last weeks of pregnancy due to fetal length or poor positioning), high birth weight, prolonged labor, breech position, abnormal intrauterine fetal positioning (descending of the fetal head during the third trimester), and uterine anomalies [6-8].
The literature states that there are 3 types of torticollis: postural, congenital muscular, and sternomastoid tumor [1], [9], that is, the baby's position can alter the movement of the muscle and this subsequently maintained alteration can be replaced by dense fibrous tissue [8].
One study found a prevalence rate of torticollis ranging from 0.3 % to 3.92 % in babies with more severe neck involvement [10]. However, another study reported a prevalence of 16 % [11], with a higher predominance on the left side [12]. Some authors report a higher prevalence of torticollis in males due to a larger head circumference and faster head growth, together with less flexibility in male fetuses [13, 14].
The limitation of cervical movement, caused by shortening of the SCM, favors contralateral cervical rotation and may lead to the development of occipital flattening. This occipital flattening, maintained by the torticollis on the opposite side, can intensify and evolve into positional plagiocephaly. Clinically, due to the decrease in muscle movement on the side of the torticollis, a tilt of the mandible may be observed, that is, greater approximation of the maxillary jaw and also of the gum line region, resulting, over time, in shortening of the mandibular branch. On the other hand, on the side opposite the torticollis there will be a change in the position of the mandibular fossa due to occipital flattening, with a consequent change in the position of the condyle and greater flexibility of muscular movement. If this pattern of movement restriction persists, the mandible becomes asymmetrical in shape and may manifest, as the baby develops, in facial asymmetries [8, 12, 15, 16].
Torticollis can also impact body development in an adaptive way. Many babies are identified with cervical imbalance after 3 months of age, from the moment they leave a horizontal position, due to head tilt. During verticalization of the body when the baby is able to sit, the head will need to be kept as centralized as possible so that there is no choking when swallowing and chewing food. The body in turn will need to adapt to this new condition; when walking, new adaptations will probably become necessary so that the baby does not lose balance [15, 17, 18].
An accurate diagnosis tool to measure facial asymmetry, focusing on the mandible, incorporating the use of ramus height proportions, could be 3D tomography, as described by some authors, demonstrating the linear measurement of the height of the ramus of the condyle to the angle of the body of the mandible [19, 20]. Histological and MRI exams can detect this tension pattern since CT scans, due to the risk of radiation to the child’s developing brain, cannot be performed for the sole purpose of evaluating mandibular asymmetry [15].
There is still no standardized tool to measure mandibular inclination [12]. Clinical examinations through visual and physical examination of the mandible and maxilla, using manual approximation between the arches were recommended and described as “the early closure of the mandible on the side affected by the torticollis while open on the contralateral side”, demonstrating that the mandible is closer to the maxila on the torticollis side [6], [12] but without objective linear measurements (Fig. 1).
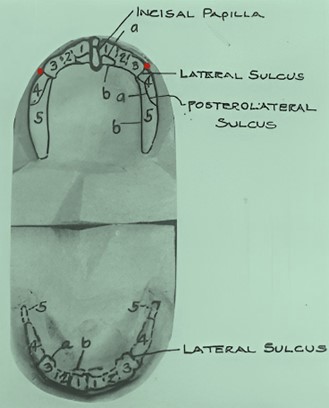
Fig. 1Observational analysis of the distance between the hemi arches, (FENTON, 2018)

In addition to the existing elements, the objective measurement of mandibular inclination , that is, this greater approximation between the dental arches, can be a tool used by dental surgeons to contribute to the diagnosis, detection and timely referral of congenital torticollis.
The current work aims to develop a measurement protocol for babies with missing teeth and another protocol for babies with incisors already present, using photogrammetry. For this protocol, two clinical cases were described.
2. Photogrammetry
2.1. Positioning on a Macri
The babies were positioned on a Macri, - (macromodelos@macromodelos.com.br), a stretcher developed for the care of babies and children. This stretcher is composed of a metal structure with an anatomical shape in the head region to allow the dentist to get closer, and a unique base that facilitates the fitting of the professional’s feet under the stretcher. The main part for attaching the child is made of rubberized fabric with a containment shirt and stabilization pillow for the head, and features metallic paint. The Macri presents some advantages: 1. Provides better comfort for the baby, making the dental procedure easier and safer for the child. 2. Easy asepsis and disinfection as it is waterproof. 3. Additional Information: Dimensions: Height 60 cm x Width 55 cm x Length 83 cm, Fabric: Courvin Odontológico and Metal, Fabric Color: Light Blue, Head support material: White Courvin, Patient age range: 0 to 4 years - (for better craniosacral stability), with Velcro for immobilization (Fig. 2).
The babies were positioned on the Macri with an inclination of 220 in relation to the ground, and a distance of 0.45 cm between the cell phone holder and the baby’s head.
Fig. 2Macri. Baby positioned at a tilt of 220 and wrapped with a Velcro band at a distance of 45 cm. Full-size photo with direct measurement from the diagonal between the baby’s lips to the center point of the cell phone holder

2.1.1. Photographic sequence
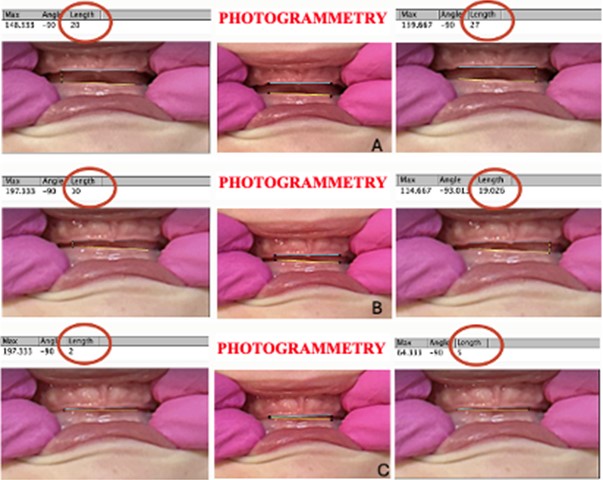
One professional positioned themself behind the baby’s head and another in front of the baby. The professional behind the baby’s head moved the lips apart with the index and ring fingers to gain access to the oral cavity. The second professional, in front of the baby, took photos, taken automatically, to record all movements: maximum mouth opening, intermediate opening (difference between maximum opening and final position) and final position (touching at least one side of the dental arches) (Fig. 3).
2.1.2. Removing the baby from the Macri and sending the photos to the computer
The baby was then removed from the Macri and placed on the mother’s lap. The photos were sent, via Airdrop, to the computer, duly cropped, using the IMAGE J program, in order to frame and center the mouth, so that photogrammetry could be carried out.
Fig. 3a) Maximum mouth opening when crying, b) intermediate mouth closure, c) final mouth closure

2.1.3. Photogrammetry
Sequential photos were taken from the beginning of the opening until the touch between the maxilla and mandible. By viewing the photos, 3 were selected: 3.A. Photo at maximum aperture, 3.B. Photo where there was touch between jaws and 3.C. In these photos, the reference points (baby with missing teeth and baby with front teeth) were marked in PowerPoint to draw two vertical lines, one on the maxilla and the other on the mandible. Objective measurements were obtained through the specific photogrammetry program using linear lines established by IMAGEJ® software (National Institutes of Health, USA). The cutoff point was considered by the researcher to represent a clinical difference in mandibular inclination between the two sides.
3. Description of cases
3.1. Baby with missing teeth
3.1.1. Reference points
The reference points were based on the location of the lateral grooves of the gingival margins and were named as reference points for anatomical assessment in the maxilla because they are consistently present in the gingival margin and are well defined, as they run anteriorly from the lingual to the labial surface and are present on the anterior margins of the first deciduous molar segments. However, in the mandible this groove can only be seen on the lingual surface [21], which is why this point on the lower gingival margin was not used in this work, but rather the projection of the upper straight line of the gingival margin (Fig. 4).
Fig. 4Location of the lateral groove (right/left side)
3.1.2. Measurement protocol for baby with missing teeth
Points were marked in the lateral grooves of the maxilla and an upper straight line was drawn. The points marked on the mandible are vertical projections of the points marked on the maxilla and a lower straight line was drawn (Fig. 5).
Fig. 5Reference points: lateral grooves of the upper gingival margin and the projection of the upper straight line of the upper edge onto the lower edge

3.1.3. Clinical case 1
A 10-month-old male baby was referred to the dental office by the physiotherapist with a report of congenital torticollis on the right side and mild plagiocephaly on the left side. The baby was born vaginally at 36 weeks, having remained engaged in the pelvis from 33 weeks of intrauterine life. He breastfed exclusively for up to 6 months, without preference for one breast, although the mother reported that the left breast always remained fuller after milking. From the sixth month onwards, the baby began to feed from a bottle.
Fig. 6Distance between the arches (right and left side) at maximum opening, intermediate, and closed positions (A, B, C,). In A, a distance of 20 pixels on the right side and 27 pixels on the left side is observed. In B, 10 pixels on the right side and 19 pixels on the left side. In C, 2 pixels on the right side and 5 pixels on the left side. There is a greater approximation of the hemimaxilla with the right hemimandible, that is, with greater inclination on the right side, the side of the torticollis
He always slept in the same position until 4 months, when the mother was advised by the physiotherapist not to support the side of the occipital bone which was slightly flattened. The baby has a history of respiratory difficulties and a nasal lavage is frequently needed to clear his nose. The parents are also accompanied by a respiratory physiotherapist.
With the aid of PowerPoint, the points in the region of the lateral grooves of the maxilla (right and left side) were marked in black. Then a straight line was drawn between these two points. To find the two points on the lower gingival margin, the two upper points were projected vertically towards the lower margins. From these two points a straight line was drawn. Using photogrammetry, the distance between the ends of the two hemiarches was measured in pixels (Fig. 6).
3.2. Baby with front teeth present (central and/or lateral incisors)
3.2.1. Reference points
The points used were between tooth/edge, with a more posterior (distal) location of the anterior region on each side (Fig. 7).
Fig. 7Baby with front teeth present. The reference used was the point determined at the distal end of the last erupting and/or erupted tooth, projected against the antagonist margin, on each side

Fig. 8Distance between the arches (right and left side) at maximum opening, intermediate, and closed positions (A, B, C,). In A, a distance of 110,510 pixels on the right side and 70,502 pixels on the left side is observed. In B, 63 pixels on the right side and 25,542 pixels on the left side. In C, 30 pixels on the right side and 10 pixels on the left side. There is a greater approximation of the hemimaxilla with the left hemimandible, that is, with greater inclination on the left side, the side of the torticollis
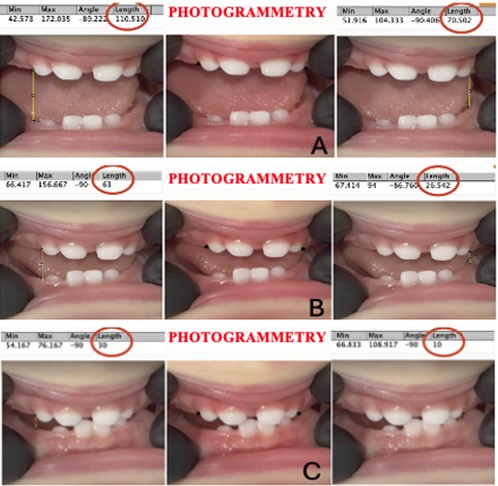
3.2.2. Clinical case 2
A male baby, 1 year and 1 month old, was referred to the dental office by the physiotherapist, with a report of congenital torticollis on the left side. The baby was born by cesarean section, at 41 weeks of intrauterine life. He breastfed exclusively and the mother reported that air escapes when expressing and the baby does not show a preference for one of the breasts. The baby has difficulty drinking water from a glass, and chokes easily. At six months the mother started introducing food.
To measure the distance between the arches, using photogrammetry, Image J was used. The vertical line started from the most anterior and distal point found, to the corresponding gingival margin on each side. The linear measurement was calculated in pixels (Fig. 8).
4. Results
It was possible to observe, through the protocol established in the present study, that there was a greater approximation between the hemi- dental arches, in the positions of maximum, intermediate and final opening, both in case 1 and case 2, on the side corresponding to the side of the torticollis. Therefore, mandibular tilt occurred on the torticollis side in both cases.
5. Discussion
The current study aimed to create a measurement protocol, through photogrammetry, between the maxilla and mandible to be used by dentists, in babies, without teeth yet erupted or with incisors already present. Two clinical cases were presented. In these two cases, the result showed greater approximation between the maxilla and mandible on the same side as the torticollis.
One of the hypotheses is that the flattening of the occipital bone on the opposite side may accentuate the approximation between the arches on the side of the torticollis. If the flattening of the occipital bone is maintained, it may cause positional plagiocephaly, altering the position of the mandibular fossa with a consequent change in the position of the condyle and facial asymmetry [8], [12], [15], [16].
This is still a proposal for a measurement protocol, using photogrammetry, as the sample includes only two cases. Studies with adequate sample sizes and comparison groups are needed to corroborate this protocol, as another diagnostic element that can be used by Pediatric Dentists or Functional Jaw Orthopedists, contributing to timely diagnosis and appropriate referral to specialized professionals.
6. Conclusions
Based on the findings of this investigation, it is suggested that objective measurement of mandibular inclination can be part of the timely diagnosis for congenital torticollis. Studies with a larger sample size should be performed to define how much of a difference in pixels means a difference between one side and the other. Appropriate methodology is necessary to confirm this diagnostic tool.
References
-
C. W. Genna, “Breastfeeding infants with congenital torticollis,” Journal of Human Lactation, Vol. 31, No. 2, pp. 216–220, Jan. 2015, https://doi.org/10.1177/0890334414568315
-
B. Sargent, S. L. Kaplan, C. Coulter, and C. Baker, “congenital muscular torticollis: bridging the gap between research and clinical practice,” Pediatrics, Vol. 144, No. 2, p. e20190582, Aug. 2019, https://doi.org/10.1542/peds.2019-0582
-
S. L. Kaplan, C. Coulter, and B. Sargent, “Physical therapy management of congenital muscular torticollis: a 2018 evidence-based clinical practice guideline from the APTA academy of pediatric physical therapy,” Pediatric Physical Therapy, Vol. 30, No. 4, pp. 240–290, Oct. 2018, https://doi.org/10.1097/pep.0000000000000544
-
A. Bashir, A. Fareeha, A. Ashfaq, A. Ayesha, and A. G. Syed, “Effect of physical therapy treatment in infants treated for congenital muscular torticollis – a narrative review,” Journal of the Pakistan Medical Association, Vol. 73, No. 1, pp. 111–116, Apr. 2022, https://doi.org/10.47391/jpma.3852
-
K. A. Golden, S. P. Beals, T. R. Littlereld, and J. K. Pomatto, “Sternocleidomastoid imbalance versus congenital muscular torticollis: their relationship to positional plagiocephaly,” The Cleft Palate-Craniofacial Journal, Vol. 36, No. 3, pp. 256–261, Dec. 2017, https://doi.org/10.1597/1545-1569_1999_036_0256_sivcmt_2.3.co_2
-
V. Wall and R. Glass, “Mandibular asymmetry and breastfeeding problems: experience from 11 cases,” Journal of Human Lactation, Vol. 22, No. 3, pp. 328–334, Jun. 2016, https://doi.org/10.1177/0890334406290096
-
L. A. van Vlimmeren, Y. van der Graaf, M. M. Boere-Boonekamp, M. P. L. ’Hoir, P. J. M. Helders, and R. H. H. Engelbert, “Risk factors for deformational plagiocephaly at birth and at 7 weeks of age: a prospective cohort study,” Pediatrics, Vol. 119, No. 2, pp. e408–e418, Feb. 2007, https://doi.org/10.1542/peds.2006-2012
-
A. A. Kuo, S. Tritasavit, and J. M. Graham, “Congenital muscular torticollis and positional plagiocephaly,” Pediatrics in Review, Vol. 35, No. 2, pp. 79–87, Feb. 2014, https://doi.org/10.1542/pir.35-2-79
-
S. Tang, Z. Liu, X. Quan, J. Qin, and D. Zhang, “Sternocleidomastoid pseudotumor of infants and congenital muscular torticollis: fine-structure research,” Journal of Pediatric Orthopaedics, Vol. 18, No. 2, pp. 214–218, Mar. 1998, https://doi.org/10.1097/01241398-199803000-00015
-
J. Von Heideken et al., “The relationship between developmental dysplasia of the hip and congenital muscular torticollis,” Journal of Pediatric Orthopaedics, Vol. 26, No. 6, pp. 805–808, Nov. 2006, https://doi.org/10.1097/01.bpo.0000235398.41913.51
-
L. Stellwagen, E. Hubbard, C. Chambers, and K. L. Jones, “Torticollis, facial asymmetry and plagiocephaly in normal newborns,” Archives of Disease in Childhood, Vol. 93, No. 10, pp. 827–831, Oct. 2008, https://doi.org/10.1136/adc.2007.124123
-
R. Fenton, S. Gaetani, Z. Macisaac, E. Ludwick, and L. Grunwaldt, “Description of mandibular improvements in a series of infants with congenital muscular torticollis and deformational plagiocephaly treated with physical therapy,” The Cleft Palate-Craniofacial Journal, Vol. 55, No. 9, pp. 1282–1288, Jul. 2018, https://doi.org/10.1177/1055665618763374
-
J. M. Graham et al., “Management of deformational plagiocephaly: repositioning versus orthotic therapy,” The Journal of Pediatrics, Vol. 146, No. 2, pp. 258–262, Feb. 2005, https://doi.org/10.1016/j.jpeds.2004.10.016
-
S. J. Bridges, “Plagiocephaly and head binding,” Archives of Disease in Childhood, Vol. 86, No. 3, pp. 144–145, Mar. 2002, https://doi.org/10.1136/adc.86.3.144
-
G. F. Rogers, A. K. Oh, and J. B. Mulliken, “The role of congenital muscular torticollis in the development of deformational plagiocephaly,” Plastic and Reconstructive Surgery, Vol. 123, No. 2, pp. 643–652, Feb. 2009, https://doi.org/10.1097/prs.0b013e318196b9be
-
C. Baumler, N. Leboucq, and G. Captier, “Study of mandibular asymmetry in plagiocephaly without synostosis,” Journal of Stomatology and Maxillofacial Surgery, Vol. 108, No. 5, pp. 424–430, Nov. 2007, https://doi.org/10.1016/j.stomax.2007.07.005
-
E. Kondo and T. J. Aoba, “Case report of malocclusion with abnormal head posture and TMJ symptoms,” American Journal of Orthodontics and Dentofacial Orthopedics, Vol. 116, No. 5, pp. 481–493, Nov. 1999, https://doi.org/10.1016/s0889-5406(99)70177-0
-
K. Urban, Z. Ignasiak, K. Wronecki, and A. Skrzek, “Change in movement patterns asymmetry in infants with central coordination disorder in continuous studies,” Biomedical Human Kinetics, Vol. 7, No. 1, Nov. 2015, https://doi.org/10.1515/bhk-2015-0023
-
L. H. Hollier, J.-H. Kim, B. Grayson, and J. G. Mccarthy, “Mandibular growth after distraction in patients under 48 months of age,” Plastic and Reconstructive Surgery, Vol. 103, No. 5, pp. 1361–1370, Apr. 1999, https://doi.org/10.1097/00006534-199904050-00004
-
G.-W. Kim, J.-H. Kim, K.-H. Lee, and H.-S. Hwang, “Reproducibility of asymmetry measurements of the mandible in three-dimensional CT imaging,” The Korean Journal of Orthodontics, Vol. 38, No. 5, p. 314, Jan. 2008, https://doi.org/10.4041/kjod.2008.38.5.314
-
J. H. Sillman, “Relationship of maxillary and mandibular gum pads in the newborn infant,” American Journal of Orthodontics and Oral Surgery, Vol. 24, No. 5, pp. 409–424, May 1938, https://doi.org/10.1016/s0096-6347(38)90295-9
About this article
The authors have not disclosed any funding.
Special thanks to Dr. Débora Lentini for sparing no effort from the beginning to the completion of this work. Thank you for your patience, attention, and above all for being such a professional, dedicated to what you set out to do.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
The authors declare that they have no conflict of interest.
The research met all applicable standards for the ethics of experimentation. Permission to carry out biomedical research was granted by CAAE of Centro Universitário Filadélfia-UNIFIL, No. 77151323.4.0000.5217, permission number 6.808.201, issue date May 07, 2024. Participants provided written informed consent prior to the study/experiment.
