Abstract
Anterior crossbite can affect primary, mixed, and permanent dentitions. Early treatment is recommended, as it can impact facial, aesthetic, functional, and developmental aspects. The etiology of anterior crossbite is multifactorial, including dental, skeletal, and postural origins. Treatment should be defined based on age and etiology, with various therapeutic resources available for correction. In primary dentition, direct flat tracks, different types of functional orthopedic appliances, quad-helix, and facial mask can be used. In mixed dentition, fixed segmented or continuous orthodontics, elastics, and other devices can be added to the treatment. In permanent dentition, orthognathic surgery may be indicated for adults, especially in cases of anterior crossbite associated with skeletal Class III that cannot be compensated dentally. This case report describes the treatment of early mixed dentition anterior crossbite with a functional orthopedic appliance at the Orthodontic Specialization, Postgraduate Course at Modal college, Belo Horizonte, Minas Gerais, Brazil. After correction, proper chewing functions were reestablished with ideal developmental stimuli.
1. Introduction
Anterior crossbite is an atypical position between the anterior teeth, in which one or more upper incisors are positioned lingually in relation to the lower incisors when in centric or habitual relation [1]. This malocclusion can be functional, dentoalveolar, or skeletal, and its etiological factors range from premature contacts, prolonged retention of deciduous teeth, and even genetic inheritance [2]. Dentoalveolar anterior crossbite occurs when the upper incisors are inclined lingually and/or the lower incisors are inclined buccally in people with Angle Class I characteristics. Skeletal anterior crossbite is linked to a Class III basal pattern, characterized by maxillary retrognathism, mandibular prognathism, or a combination of both. Functional anterior crossbite, also known as pseudo-Class III, occurs when there is interference of dental occlusion, forcing the mandible to deviate to achieve maximum intercuspation. In centric relation, the incisors are in end-to-end relationship with the molars separated, but in Class I molar relationship [3].
The prevalence of anterior crossbite can vary from 7.6 % in children, with approximately 1 % of children between two and six years old affected [4]. In Brazil, the prevalence varies from 3.3 % to 18.5 %. A study conducted in Latin American populations showed an incidence of 5 %. In studies of the Asian population, a higher incidence was observed, ranging from 9 % to 19 %, with a prevalence of around 16.7 % in Koreans [5, 9].
Numerous etiological causes have been identified to explain the development of dentoalveolar anterior crossbite, including prolonged retention of deciduous teeth, presence of supernumerary teeth, and occurrence of trauma with displacement during the deciduous dentition [8]. There are infinite possible combinations of dental, skeletal, and facial arrangements that can be characterized by the same molar relationship. It is necessary to better characterize the degree of compromise of the components that result in a certain dental, skeletal, and facial arrangement [10]. It is possible to diagnose anterior dental crossbite in the mixed dentition phase through routine general clinical exams. It is up to the general clinician to identify, diagnose, and even intercept this malocclusion. Differential diagnosis between skeletal and dental anterior crossbites is based on the inclination of the involved teeth, the relationship of the bone bases, and changes in the patient’s profile [7].
Once diagnosed, anterior crossbites should be treated as early as possible, as this type of malocclusion does not self-correct with age, but rather tends to worsen. The worsening of this type of malocclusion can result in traumatic occlusion, tooth wear facets, changes in the periodontium such as gingival recession and mobility in the involved lower incisors, temporomandibular dysfunction, as well as aesthetic damage [7, 8].
When treated early, anterior crossbites can prevent or reduce the damage caused by abnormal growth of the bone and dental bases, avoiding future periodontal problems, especially in the anterior teeth, and preventing the appearance of harmful habits such as bruxism and the development of skeletal crossbites [6]. There are several possibilities for treating anterior crossbites. Various devices, fixed or removable, can be used to correct anterior crossbite. In the orthodontic literature, authors agree that maxillary protraction, with or without rapid palatal expansion, is the best therapy for growing patients. Different types of devices used as extraoral anchorage for maxillary protraction have been described, such as the Delaire facial mask, the Petit facial mask, the Turley facial mask, and the Sky Hook, among others [9]. Another option would be the use of removable appliances with a protraction arch, which has been shown to be effective in the treatment of anterior crossbites, allowing the unlocking of the maxilla for more harmonious growth of the bone bases. They are commonly composed of retention clasps and acrylic, with a Progeny or Eschler arch, which is placed to prevent mandibular protrusion and/or to lingualize the lower incisors. Frontal palatal springs are also adapted to buccalize the upper incisors [11].
This study aims to present, through a clinical case report, the early treatment of anterior crossbite using a functional orthopedic appliance.
2. Clinical case description
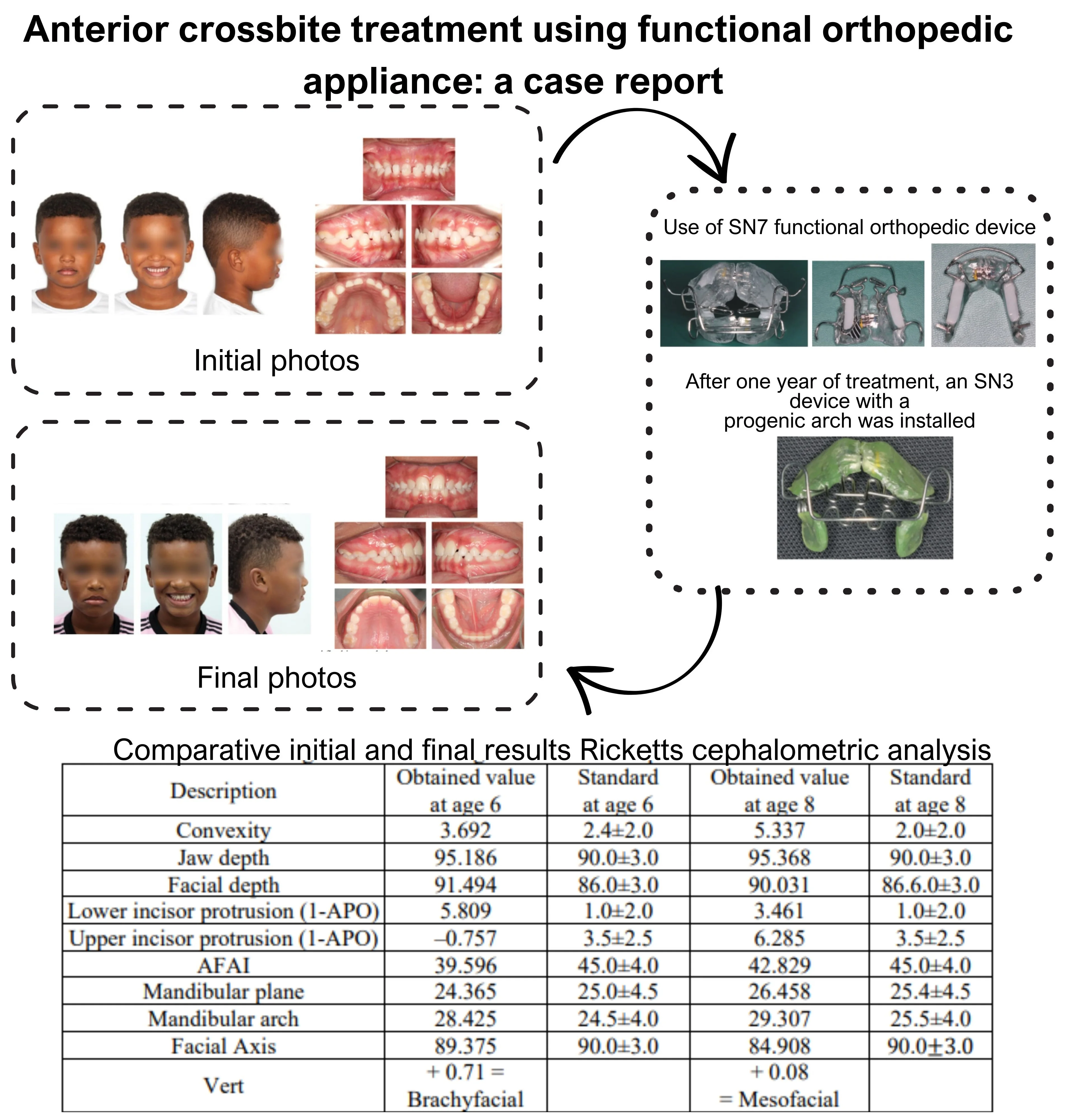
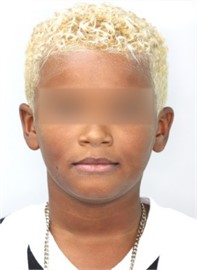
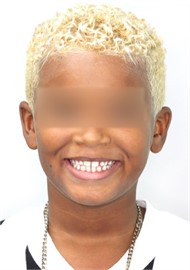
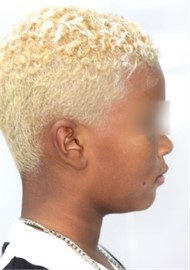
A six-year-old male patient accompanied by a guardian visited the orthodontic clinic at Faculdade Modal, Belo Horizonte, Minas Gerais, Brazil, with the main complaint of inverted incisor positioning. Orthodontic documentation was requested to make a more precise diagnosis: panoramic X-ray to assess the presence of germs on the permanent teeth and identify any alteration, profile teleradiography with cephalometric tracing for vertical and sagittal dental and skeletal evaluation, plaster models to calculate the dental discrepancy, extraoral photographs to identify asymmetries, profile classification and facial typology, as well as intraoral photographs to identify malocclusion. Frontal facial clinical analysis showed facial symmetry, lip seal at rest, proportional facial thirds with facial width proportionally increased in relation to height (Fig. 1(a)). On the lateral facial clinical analysis, good vertical balance was observed between the middle and lower thirds, with lips projected anteriorly, with the lower lip more forward than the upper lip (Fig. 1(b)). The smile evaluation showed an inverted smile, with the upper and lower midlines slightly deviated and the upper midline coinciding with the median sagittal plane (Fig. 1(c)). The dental arch analysis revealed that the patient had Class III malocclusion, with anterior and deep crossbite (Figs. 1(d-f)). The model discrepancy was positive, with the presence of several diastemas in both the upper and lower arches (Figs. 1(g-h)). The patient was in the first transitional period of dentition, with eruption of the lower central incisors (31 and 41) and presence of the first upper and lower molars (16, 26, 36, and 46). The panoramic radiography showed a normal pattern with condylar symmetry, the presence of all deciduous teeth and permanent dental germs that will erupt later in the oral cavity, except for the third molars. All teeth and periodontal structures presented normal conditions (Fig. 2). The lateral cephalometric radiograph showed tonsils, adenoids, and paranasal sinuses within normal limits, low tongue, satisfactory airways, and phase 1 vertebral growth (Fig. 3). A Lavergne-Petrovic cephalometry was performed, classifying the patient in the rotational group P1N, and in the lateral Ricketts analysis, an anterior mandibular positioning and altered incisor inclinations were observed (Table 1).
Fig. 1Initial photos: a) frontal extraoral photo; b) profile extraoral photo; c) smiling frontal extraoral photo; d) frontal intraoral photo; e) right lateral intraoral photo; f) left lateral intraoral photo; g) upper occlusal intraoral photo; h) lower occlusal intraoral photo

a)

b)

c)

d)

e)

f)

g)

h)
Table 1Ricketts cephalometric analysis performed on December 2, 2020
Description | Obtained value | Standard |
Convexity | 3.692 | 2.4±2.0 |
Jaw depth | 95.186 | 90.0±3.0 |
Facial depth | 91.494 | 86.0±3.0 |
Protrusion of lower incisor (1-APO) | 5.809 | 1.0±2.0 |
Protrusion of the upper incisor (1-APO) | –0.757 | 3.5±2.5 |
AFAI | 39.596 | 45.0±4.0 |
Mandibular plan | 24.365 | 25.0±4.5 |
Mandibular arch | 28.425 | 24.5±4.0 |
Facial axis | 89.375 | 90.0±3.0 |
Vert: 0.71 = Brachyfacial |
A measurement of the total convexity of the face was also taken and a value of 174° was found, where 165° to 175° is considered a straight profile. However, for the patient's age and race, it should be a lower value (Fig. 4).
Fig. 2Initial panoramic X-ray

Fig. 3Initial lateral cephalometric radiograph
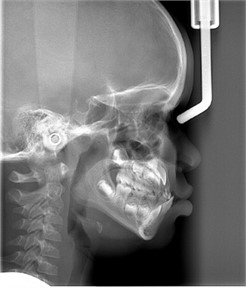
Fig. 4Profile convexity angle
2.1. Treatment
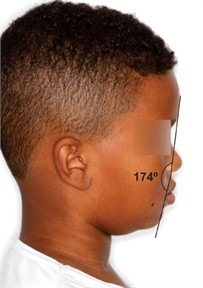
The initial objective of the intervention was to remove the occlusal interferences in centric relation that kept the mandible in a more anterior position (Fig. 5(a)). Often, small occlusal adjustments are necessary, mainly in the region of the deciduous canines (Figs. 5(b-d)). Treatment began with these small occlusal adjustments (Fig. 5(e)) and the installation of a functional orthopedic appliance, SN7 (Figs. 6(a-c)).
Fig. 5Occlusal interferences: a) interference in centric occlusion; b) carbon marks of the interferences; c) carbon marks of the interferences; d) carbon marks of the interferences; e) wear for removal of the interference

a)

b)

c)

d)

e)
This appliance was presented by Dr. Wilma Simões, indicated for mesioclusion, and chosen to change the mandibular posture and promote anterior uncrossing (Figs. 7(a-c)). The upper frontal springs will be very important to stimulate the vestibularization of the upper incisors during their eruption, to obtain the correct overjet (Fig. 7(d)). In the lower appliance, the acrylic should be kept away from the lingual faces of the lower incisors to allow for retroclination with the adjustment of the vestibular arch and to assist in anterior uncrossing (Fig. 7(e)). Six months after the start of treatment, the patient already has a much better and more stable posture, with the incisors still in the process of eruption (Fig. 8(a-c)). However, total eruption of the incisors, with correct vertical and horizontal overlap, is necessary for ideal stability. After two more months of appliance use (Figs. 9(a-e)), we can already observe positive overbite and overjet (Figs. 10(a-d)). Changes in the smile, profile, and lip posture are clear in the patient's face (Figs. 10(e-g)). After one year of treatment, a new panoramic control X-ray was requested (Fig. 11), where we can already observe the imminent eruption of the upper lateral incisors in the oral cavity, which can also be observed clinically (Fig. 12(a-c)). We decided to replace the appliance in order to monitor the eruption of the lateral incisors and at the same time work on better lingual posture. The SN3 appliance with a progenic arch was installed (Figs. 13(a-d)). A new lateral cephalometric radiograph was taken to evaluate the changes with the treatment (Fig. 14). In the cephalometric values found, we can observe changes in the position of the mandible and the inclination of the incisors (Table 2).
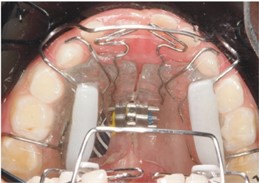
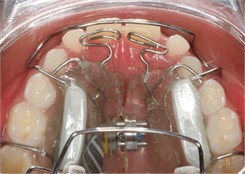
Fig. 6SN7 brace: a) SN7 in occlusion; b) superior occlusal view of SN7; c) inferior occlusal view of SN7

a)

b)
c)
Fig. 7Adapted SN7 brace: a) frontal intraoral photo with SN7; b) right lateral intraoral photo with SN7; c) left lateral intraoral photo with SN7; d) upper occlusal intraoral photo with SN7; e) lower occlusal intraoral photo with SN7

a)

b)

c)
d)
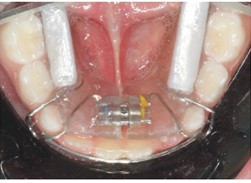
e)
Fig. 8Intraoral photos six months after the start of treatment: a) right intraoral photo; b) front intraoral photo; c) left intraoral photo

a)

b)

c)
Fig. 9Intraoral photos with SN7 eight months after the start of treatment: a) frontal intraoral photo; b) right lateral intraoral photo; c) left lateral intraoral photo; d) occlusal superior intraoral photo; e) occlusal inferior intraoral photo

a)

b)

c)
d)
e)
Fig. 10Photos eight months after treatment initiation: a) front intraoral photo; b) right lateral intraoral photo; c) left lateral intraoral photo; d) overbite intraoral photo; e) frontal extraoral photo; f) smiling frontal extraoral photo; g) profile extraoral photo

a)

b)

c)

d)
e)
f)
g)
Fig. 11Panoramic X-ray 1 year after treatment initiation

Fig. 12Intraoral photos one year after the start of treatment: a) frontal intraoral photo; b) right lateral intraoral photo; c) left lateral intraoral photo

a)

b)

c)
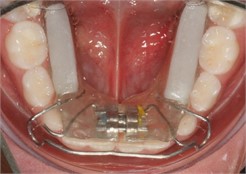
Fig. 13SN3 photos: a) frontal view; b) intraoral front view with SN3; c) intraoral right lateral view with SN3; d) intraoral left lateral view with SN3

a)

b)

c)

d)
Fig. 14Lateral cephalometric radiograph one year and three months after the start of treatment

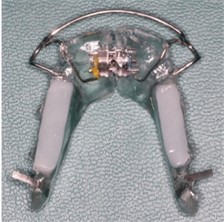
Table 2Comparison between Ricketts cephalometric analyses performed at different times during treatment (initial and one year and six months after the start), where it was possible to observe positive changes achieved through functional orthopedic treatment.
Description | Obtained value at age 6 | Standard at age 6 | Obtained value at age 8 | Standard at age 8 |
Convexity | 3.692 | 2.4±2.0 | 5.337 | 2.0±2.0 |
Jaw depth | 95.186 | 90.0±3.0 | 95.368 | 90.0±3.0 |
Facial depth | 91.494 | 86.0±3.0 | 90.031 | 86.6.0±3.0 |
Lower incisor protrusion (1-APO) | 5.809 | 1.0±2.0 | 3.461 | 1.0±2.0 |
Upper incisor protrusion (1-APO) | –0.757 | 3.5±2.5 | 6.285 | 3.5±2.5 |
AFAI | 39.596 | 45.0±4.0 | 42.829 | 45.0±4.0 |
Mandibular plane | 24.365 | 25.0±4.5 | 26.458 | 25.4±4.5 |
Mandibular arch | 28.425 | 24.5±4.0 | 29.307 | 25.5±4.0 |
Facial Axis | 89.375 | 90.0±3.0 | 84.908 | 90.0 |
Vert | + 0.71 = Brachyfacial | + 0.08 = Mesofacial |
After five months of use, this appliance was sufficient to complete the eruption of the lateral incisors. After one year and seven months from the beginning of the treatment, the patient was discharged without the use of any type of retention appliance, as this will be maintained by the re-established oral functions.
Fig. 15Final photos taken one year and seven months after the start of treatment: a) final frontal extraoral photo; b) final extraoral smile frontal photo; c) final profile extraoral photo; d) final intraoral front photo; e) final intraoral right lateral photo; f) final intraoral left lateral photo; g) final angled intraoral right lateral photo; h) final angled intraoral left lateral photo; i) final intraoral superior occlusal photo; j) final intraoral inferior occlusal photo

a)

b)

c)

d)

e)

f)

g)

h)

i)

j)
Final photos show facial changes (Figs. 15(a-c)) as well as correction of Class III and anterior crossbite with great occlusal stability (Figs. 15(d-j)). A comparison between the face at the beginning and end of treatment (Fig. 16) and occlusal changes (Fig. 17) are also shown.
Fig. 16Initial and final extraoral photos

Fig. 17Initial and final intraoral photos

3. Discussion
Authors agree that the etiology of anterior crossbite is multifactorial, resulting from a maxillomandibular discrepancy, usually due to a well-developed mandible, a poorly developed maxilla, or in some situations, a combination of both factors. Some other dental factors may also contribute to anterior crossbite, such as trauma to the deciduous dentition, retention of deciduous incisors, early loss of deciduous incisors, supernumerary teeth, cysts, tumors, among others. Oral habits such as interposition of the upper lip can also alter the inclination of the upper incisors, leading them to a more palatal position [1], [11-12].
Anterior crossbite is a malocclusion that affects individuals psychologically and aesthetically. The diagnosis should be made early so that individuals with this anomaly can be followed from childhood. Interceptive orthodontics is the orthodontic approach applied in deciduous or mixed dentition with the main objective of promoting the development of a favorable occlusion, correcting the dentofacial alterations in their initial phases. It allows for the early correction of anterior crossbite, promoting the harmonious growth of the bone bases and, if possible, restoring normal occlusion and more balanced facial growth. One of the alternatives for the treatment of anterior crossbite is the use of removable appliances [13-15] as well as the use of a facial mask associated or not with palatal expansion [16].
Orthopedic treatments for Class III with anterior crossbite seek to improve the profile by advancing the maxilla [17] and rotating the mandible clockwise, which may be anteriorized as a result of condylar growth or anterior displacement of the condyle in the mandibular fossa [18-20].
In mixed dentition, the individual undergoes the greatest morphological transformations, making it important to use the correct interceptive procedures. It is also necessary to make it clear to the patient and responsible parties that this treatment requires a lot of cooperation and may exceed the normal period of conventional orthodontic therapy, as it is a process in which the patient's growth and development are observed and followed [21-22].
There are several functional orthopedic appliances for use in the treatment of anterior crossbite. Early diagnosis of the problem is necessary to obtain good results. Functional orthopedics of the jaws helps to stimulate facial structures and establish a harmonious development of the stomatognathic system, especially in patients in mixed dentition with a diagnosis of anterior crossbite. We must also emphasize that the indication of functional orthopedic appliances depends on an efficient diagnosis with cephalometric analysis, facial analysis, model analysis, thorough clinical examination, as well as identification of the patient's bone age. It is also important to eliminate possible harmful habits and parafunctions, in order to guarantee the success and stability of the treatment [8], [22-23].
Appliances with a pro-growth arch assist in the effective interceptive treatment of dentoalveolar anterior crossbite, promoting a quick and effective correction, with little discomfort for the patient and easy clinical management [13]. This type of appliance aims to alter the rotation of mandibular growth, promoting a change in the maxillomandibular posture. The lateral pterygoid, digastric, and styloglossus muscles, when stimulated, modulate the bones and properly position the teeth in the arch [23].
Since it does not require dental anchorage, jaw functional orthopedics offers therapeutic resources for controlling this malocclusion at an opportune age, making it possible and mandatory to correct anterior crossbite regardless of the type of mesial occlusion that the patient presents. Additionally, correcting Class III malocclusion during deciduous dentition will lead to correct stimuli for the harmonious development of the maxillary facial complex. There is much discussion about the effectiveness of treating Class III malocclusion at an appropriate age, always seeking stability, but most authors have studied the use of facial masks, with few using functional orthopedic appliances in their studies [24].
4. Conclusions
Anterior crossbite correction should be performed as early as possible and functional orthopedic appliances can be used when well indicated. More high-quality studies are needed to evaluate the best options for early treatment of this malocclusion.
References
-
S. Gallão, L. P. Martins, K. Faltin Junior, L. V. Pieri, A. M. M. Gaspar, and P. D. A. Bolini, “Diagnóstico e tratamento precoce da classe III: relato de caso clínico,” Journal of the Health Sciences Institute, Vol. 31, No. 1, 2013.
-
M. S. Vianna, F. A. Casagrande, E. S. Camargo, and J. H. G. Oliveira, “Mordida cruzada anterior: relato de um caso clínico,” Jornal Brasileiro de Ortodontia e Ortopedia Facial, Vol. 8, No. 44, pp. 99–109, 2003.
-
Sule Bayrak and Emine Sen Tunc, “Treatment of anterior dental crossbite using bonded resin-composite slopes: case reports,” European Journal of Dentistry, Vol. 2, No. 2, p. 303, Oct. 2008.
-
M. E. C. Almeida, M. Vedovello Filho, S. A. S. Vedovello, A. Lucatto, and A. T. Torrezan, “Prevalência de má oclusão em escolares da rede estadual do município de Manaus, AM – Brasil,” Revista Gaúcha de Odontologia, Vol. 55, No. 4, pp. 389–394, 2007.
-
L. S. Lopes and M. C. T. Cangussu, “Prevalência e severidade das alterações oclusais em escolares,” Revista de Ciências Médicas e Biológicas, Vol. 4, No. 2, pp. 105–112, 2005.
-
A. Y. Tashima, A. P. Verrastro, S. L. M. Ferreira, M. T. Wanderley, and E. G. Pinto, “Tratamento ortodôntico precoce da mordida cruzada anterior e posterior: relato de caso clínico,” Jornal Brasileiro de Odontopediatria and Odontologia do Bebê, Vol. 6, No. 29, pp. 24–31, 2003.
-
Luciane Monte Alto de Seabra, Nathália Lima Freze Fernandes, R. Lira, D. Souto, Loana Paula de Oliveira, and Debora Medina, “Mordida cruzada anterior: possibilidades de tratamento na dentição decídua e mista,” Revista Naval de Odontologia, Vol. 46, No. 1, pp. 59–68, 2019.
-
A. C. S. Salles, M. M. Pereira, T. C. Marinho, Z. M. A. Faria, G. E. R. Queiroz, and J. C. Avelar, “Mordida cruzada anterior: diagnóstico e etiologia; relato de caso,” in FAVE, 2020.
-
A. P. R. Perrone and J. N. Mucha, “O tratamento da Classe III: revisão sistemática – Parte I. Magnitude, direção e duração das forças na protração maxilar,” Revista Dental Press de Ortodontia e Ortopedia Facial, Vol. 14, No. 5, pp. 109–117, Oct. 2009, https://doi.org/10.1590/s1415-54192009000500015
-
W. J. S. Ursi and M. Matias, “Surgical-orthodontic treatment of a young patient with dentofacial deformity due to maxillary deficiency and mandibular excesso,” Clinical Orthodontics, Vol. 21, No. 4, pp. 114–124, 2022.
-
A. Ulusoy and E. Bodrumlu, “Management of anterior dental crossbite with removable appliances,” Contemporary Clinical Dentistry, Vol. 4, No. 2, p. 223, 2013, https://doi.org/10.4103/0976-237x.114855
-
P. B. A. Figueiredo, R. P. Ferraz, V. C. Silva, J. M. Pinheiro Junior, A. R. Q. D. Silva, and A. I. Silva, “Plano inclinado no tratamento da mordida cruzada anterior: relato de caso clínico,” Revista da Faculdade de Odontologia, Vol. 19, No. 2, pp. 229–233, Aug. 2014.
-
R. A. Moura, A. H. M. Simplício, M. J. C. C. Lau, A. N. S. Amorim, F. A. J. C. Silva, and M. V. Melo Neto, “Use of the modified progenic apparatus in the previous cross-bite interception,” Research, Society and Development, Vol. 9, No. 8, 2020.
-
L. F. C. Tocci, O. G. D. Silva Filho, A. Fuziy, and J. R. P. Lauris, “Influence of intentional ankylosis of deciduous canines to reinforce the anchorage for maxillary protraction,” Dental Press Journal of Orthodontics, Vol. 18, No. 1, pp. 94–102, Feb. 2013, https://doi.org/10.1590/s2176-94512013000100020
-
H. S. A. Matos, “Anomalia de classe III,” Universidade Fernando Pessoa, Faculdade Ciências da Saúde, Porto, 2014.
-
M. Foersch, C. Jacobs, S. Wriedt, M. Hechtner, and H. Wehrbein, “Effectiveness of maxillary protraction using facemask with or without maxillary expansion: a systematic review and meta-analysis,” Clinical Oral Investigations, Vol. 19, No. 6, pp. 1181–1192, Jul. 2015, https://doi.org/10.1007/s00784-015-1478-4
-
U. E. M. Schneider-Moser and L. Moser, “Very early orthodontic treatment: when, why and how?,” Dental Press Journal of Orthodontics, Vol. 27, No. 2, 2022, https://doi.org/10.1590/2177-6709.27.2.e22spe2
-
J. C. Voudouris, D. G. Woodside, G. Altuna, M. M. Kuftinec, G. Angelopoulos, and P. J. Bourque, “Condyle-fossa modifications and muscle interactions during Herbst treatment, Part 1. New technological methods,” American Journal of Orthodontics and Dentofacial Orthopedics, Vol. 123, No. 6, pp. 604–613, Jun. 2003, https://doi.org/10.1016/s0889-5406(03)00149-5
-
J. C. Voudouris, D. G. Woodside, G. Altuna, G. Angelopoulos, P. J. Bourque, and C. Y. Lacouture, “Condyle-fossa modifications and muscle interactions during Herbst treatment, Part 2. Results and conclusions,” American Journal of Orthodontics and Dentofacial Orthopedics, Vol. 124, No. 1, pp. 13–29, Jul. 2003, https://doi.org/10.1016/s0889-5406(03)00150-1
-
A. B. Rodriguez, M. M. Uribe, C. A. Morales, and C. H. Martínez-Cajas, “Tratamento precoce de más-oclusões esqueléticas de Classe II – comparação de três aparelhos ortopédicos funcionais: Bionator, Klammt, SN1,” Ortodontia, Vol. 46, No. 6, pp. 20–30, 2014.
-
P. V. P. Oltramari, D. G. Garib, A. C. C. F. Conti, J. F. C. Henriques, and M. R. Freitas, “Tratamento ortopédico da Classe III em padrões faciais distintos,” Revista Dental Press de Ortodontia e Ortopedia Facial, Vol. 10, No. 5, pp. 72–82, Oct. 2005, https://doi.org/10.1590/s1415-54192005000500008
-
B. S. Veras, L. A. Padial, M. G. O. Lopes, and E. B. Shinozaki, “Utilização dos aparelhos ortopédicos no tratamento das más oclusões de classe II e III; uma revisão da literatura,” in 16th Encontro Latino-Americano de Iniciação Científica e XII Encontro Latino-Americano de Pós-Graduação, 2012.
-
F. M. Callado and M. L. Sperandeo, “Anterior crossbite correction in early mixed dentition stage using functional jaw orthopedics principles: a case report with two-years follow-up,” Jaw Functional Orthopedics and Craniofacial Growth, 2021.
-
M. R. Xavier Sancho Rios, A. Alves de Carvalho, A. Silveira Martins, A. Souza Nery, and M. A. Drummond, “Jaw functional orthopedics is a therapeutic alternative for class III malocclusion: a case report,” Jaw Functional Orthopedics and Craniofacial Growth, Vol. 1, No. 2, pp. 44–53, Dec. 2021, https://doi.org/10.21595/jfocg.2021.22059
Cited by
About this article
The authors have not disclosed any funding.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Vilmara Geralda Francisco de Assis: conceptualization, data curation, methodology, project administration, supervision, visualization, writing – original draft preparation, writing – review and editing. Saulo Gribel: conceptualization, data curation, investigation, methodology, project administration, resources, writing – original draft preparation, writing – review and editing. Anderson Mamede: conceptualization, data curation, software, writing – original draft preparation, writing – review and editing.
The authors declare that they have no conflict of interest.
The research met all applicable standards for the ethics of experimentation. According to resolution No. 466, there is no need for approval of the research by the ethics committee. Participants provided written informed consent prior to the study.
