Abstract
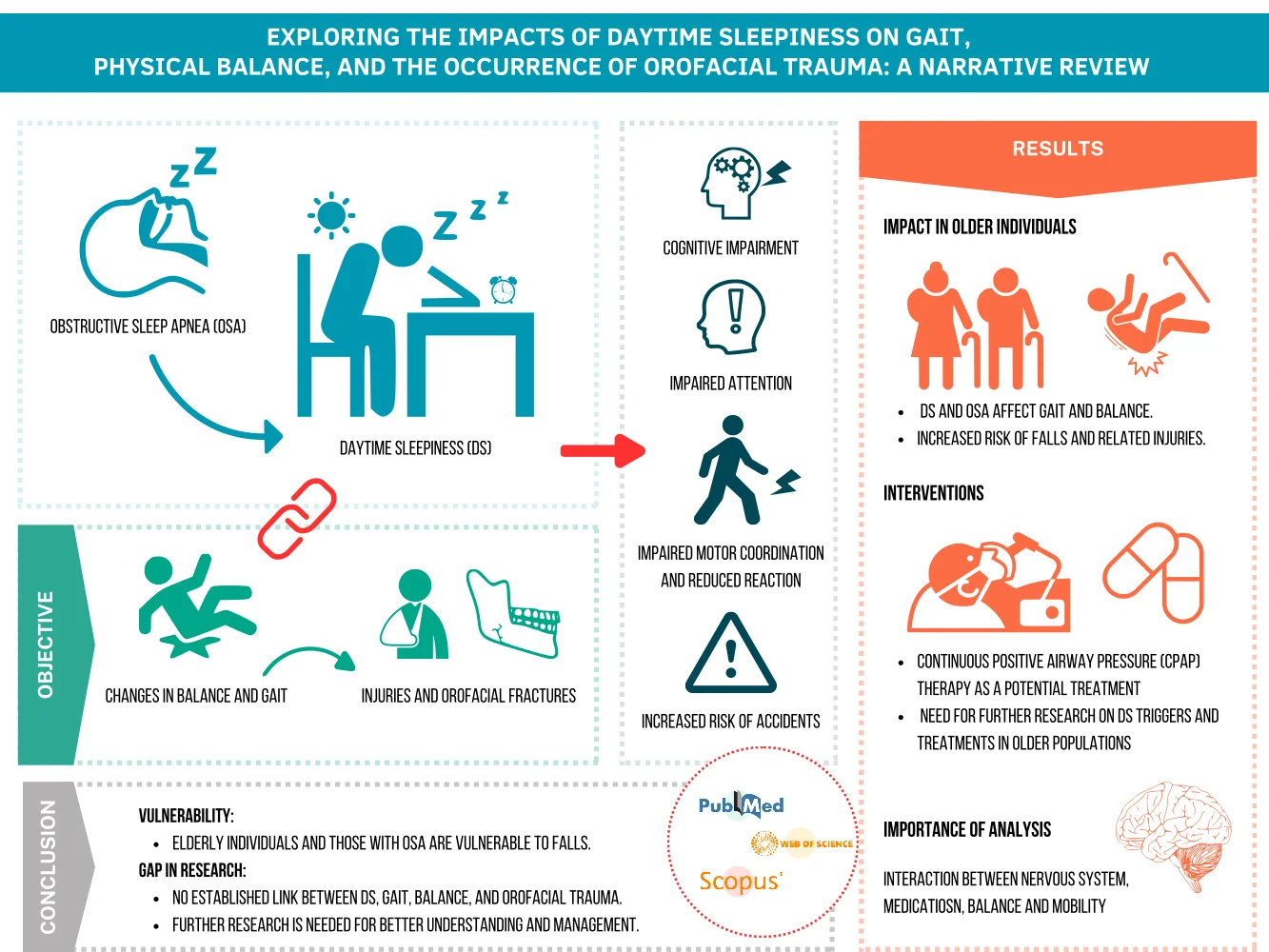
Daytime sleepiness (DS) often accompanies obstructive sleep apnea (OSA), exacerbating its effects. DS can impair cognitive function, attention, reaction time, and motor coordination, increasing the risk of accidents. This study aimed to explore the relationship between DS, changes in gait and balance, and the occurrence of orofacial fractures. A narrative review was conducted using PubMed, Scopus, and Web of Science publications. The analysis revealed the impact of DS and OSA on gait and balance control in older individuals, emphasizing the need for interventions to address these issues and identify associated pathologies. Continuous Positive Airway Pressure (CPAP) therapy was recognized as a potential treatment, although further research is needed to understand DS triggers and treatment options in older populations. The study underscores the importance of analyzing interactions between the central nervous system, medications, balance, and mobility to prevent falls and related injuries. While the literature highlights the vulnerability of elderly individuals and those with OSA to falls, no established link between DS, gait, balance, and orofacial trauma necessitating medical and dental intervention was found. Thus, further research is warranted to address this gap and promote better understanding and management of these conditions.
Highlights
- Daytime sleepiness, frequently associated with obstructive sleep apnea, significantly affects cognitive function, attention, reaction time, and motor coordination, raising the risk of accidents.
- CPAP therapy shows promise in treating Daytime Sleepiness, though more research is needed to validate its effectiveness in older populations.
- Daytime sleepiness impacts gait and balance in older adults, increasing the risk of falls and associated injuries.
- There's a critical need for studies on the interplay between central nervous system, medications, balance, and mobility to prevent falls and related injuries.
1. Introduction
Daytime sleepiness, characterized by difficulty maintaining wakefulness and alertness during typical waking hours, emerges as a significant public health challenge [1], impacting quality of life, especially in adults [2]. This complex phenomenon is associated with an interaction between psychological factors, sleep habits, lifestyle, lack of physical activity, and dietary choices [3]. Its influence on sleep quality interferes with daily activities, performance at work or studies, and social relationships [4]. Therefore, cognitive impairment, translated into difficulty concentrating, poor memory, and reduced performance in intellectual tasks [5], can increase the risk of accidents, especially in activities that require attention [4], such as driving and operating cutting machines. In Finland, the frequency of DS occurring daily or almost daily is most often associated with depression, insomnia, and sleep-disordered breathing (SDB), accounting for a total of 11.0 % of women and 6.7 % of men [3].
Excessive daytime sleepiness (EDS) can also be associated with underlying medical conditions such as sleep disorders, thereby contributing to long-term health problems [6]. It has an estimated prevalence of 2.5 % to 18.5 % in the general population and is more common in women than men [7]. EDS is characterized by difficulty in remaining awake and alert during the main waking episodes of the day, with sleep occurring involuntarily or at inappropriate times during the waking period [8]. In China, EDS has been significantly associated with cognitive dysfunction in young and middle-aged patients with obstructive sleep apnea (OSA) [6]. Not only does it significantly impact the health of affected individuals, but it also threatens public safety [9].
Recent studies have shown that balance and gait abnormalities in OSA can be explained by factors such as nocturnal hypoxemia, sleep fragmentation, cognitive impairment, neuromuscular changes, and the impact on sleep quality [10, 11]. These elements affect coordination and stability during gait, increasing the risk of falls [11]. Other studies mention that balance, posture, and gait abnormalities resulting from DS can be explained by several mechanisms, including sleep pattern disruption, reduced cognitive alertness, changes in neuromuscular control, and muscle fatigue [10, 11]. These factors compromise motor coordination and increase the risk of falls during physical activity [11].
This article addresses the gap in DS research, investigating its potential influence on gait characteristics and its implications on balance, especially regarding the risk of orofacial fractures. It was hypothesized that DS, by compromising sleep quality and influencing breathing patterns, can trigger changes in gait and balance, thereby increasing the risk of traumatic events.
Investigating this possible connection has significant implications for comprehensively understanding the impacts of DS on human gait and orofacial trauma. Additionally, it can provide actionable insights for healthcare professionals, highlighting the importance of integrated assessments and preventive strategies in patients with this disorder.
2. Methods
This qualitative narrative review investigates the influence of daytime sleepiness on gait and balance characteristics in the adult population, as well as on orofacial trauma. Data collection took place between February and March 2024, using the PubMed, Scopus, and Web of Science databases, employing MeSH terms in the following query: “(((daytime sleep*) OR (respiratory sleep disorders*)) AND (gait)) AND (Physical balance)”. We used MeSH terms to select only articles focused on our research objective. The chosen articles had to be original or peer-reviewed and in English. Initially, nine articles were identified during indexing, considering their titles and abstracts. After analyzing the abstracts, two articles were selected. Subsequently, two independent researchers double-checked and selected these two articles for inclusion in this study. Publications were excluded for describing single cases, rare diseases, syndromes, patient subgroups, treatment procedures, or articles in languages other than English. After carefully selecting the articles, a series of steps were carried out: exploratory reading, selection of material aligned with the study’s objectives, analysis of the text, and interpretative reading that preceded the writing process.
3. Results
Two articles were selected based on the search criteria for inclusion in this review (see Table 1). One of these articles described an observational cohort study investigating the relationship between sleepiness and balance measures in older adults living in the community [10]. The main study lasted one year and included 120 participants, aged 78.2 years on average, who attended clinical appointments at baseline, 6 months, and 12 months [10]. A secondary analysis used data from baseline assessments of 116 participants who completed the Epworth Sleepiness Scale (ESS) to evaluate daytime sleepiness. Additionally, the study examined the association between self-reported daytime sleepiness and mobility/balance in this population, suggesting a negative correlation with gait speed, performance-based balance measures, and subjective confidence in balance. The study also investigated the potential influence of medication use on these associations within the population [10].
The second article consisted of a narrative review and discussion on the relationship of obstructive sleep apnea on balance/gait and the risk of falls. In addition, it investigated the efficacy of Continuous Positive Airway Pressure therapy in improving markers of fall risk. It outlined potential mechanisms by which OSA may contribute to balance/gait impairments [11].
The case studies presented in Table 1 investigated the effects of DS and sleep-disordered breathing (SDB) on gait, balance, and the risk of falls in adults. These studies highlighted the importance of early identification of these associations for implementing appropriate interventions to improve sleep quality and locomotor function.
Table 1This table displays the two selected articles, arranged in descending order of citations, that investigated the association between daytime sleepiness, gait, and balance.
Ranking | Type of study | Article | No. of citations |
1 | Cohort | Tyagi S, Perera S, Brach JS. Balance and mobility in community-dwelling older adults: effect of daytime sleepiness. J Am Geriatr Soc. 2017 May;65(5):1019-1025 [10] | 25 |
2 | Review | Stevens D, Jackson B, Carberry J, McLoughlin J, Barr C, Mukherjee S, Oh A, McEvoy RD, Crotty M, Vakulin A. The impact of obstructive sleep apnea on balance, gait, and falls risk: a narrative review of the literature. J Gerontol A Biol Sci Med Sci. 2020 Nov 13;75(12):2450-2460 [11] | 24 |
3.1. The possible effects of daytime sleepiness on balance and mobility
Daytime sleepiness has been consistently correlated with variables that directly influence gait and balance [10]. This study, published in 2017, showed a significant association between self-reported DS, a slower gait speed, and low balance confidence in community-dwelling older adults. Moreover, it stressed that subjective sleep assessment should be considered when evaluating balance and implementing interventions to improve balance in older adults. Therefore, it emphasized the need for further research to identify potential contributors to DS, such as insomnia or sleep apnea, and to examine the effect of treating these conditions on mobility. Furthermore, the study highlighted the importance of delving deeper into the complex interactions involving the central nervous system, medication use, balance, and mobility [10].
3.2. The possible impacts of sleep-disordered breathing on balance, gait, and risk of falls
This review study [11] investigated the relationship between obstructive sleep apnea (OSA) and balance, gait, and the risk of falls. It was reported that increasing rates of hospitalization [12] and fall-related injuries are a global concern, primarily due to the aging population and associated health problems that increase the risk of falls [11]. One of these health problems is OSA, a common disorder characterized by repeated obstruction or cessation of airflow during sleep. Additionally, some analyzed studies [11] mentioned that subjective sleep quality and the presence of OSA are associated with a higher risk of falls. Therefore, mechanistic studies are needed to understand how OSA can affect posture, balance, and gait, mainly due to nocturnal hypoxemia, a common consequence of OSA [11].
Furthermore, it was mentioned that although treating OSA with continuous positive airway pressure (CPAP) may improve gait, its impact on posture and balance remains uncertain. Moreover, the complexity of balance control was emphasized, involving various physiological systems such as vestibular, muscular, visual, and cognitive, all potentially affected by OSA. Additionally, it was mentioned that nocturnal hypoxic burden plays an essential role in this impact on posture and balance. Therefore, future large-scale randomized controlled trials are needed to determine the efficacy of OSA treatment in reducing the risk of falls [11].
The analyzed cohort and review studies examined the effects of DS and sleep-related breathing disorders, indicating a potential association with changes in motor coordination, balance, and increased risk of falls. However, despite these concerns, no direct link was found to establish the influence of these associations on the incidence of events such as orofacial fractures and, consequently, hospitalization and dental surgical interventions. This suggests a gap in the theme, highlighting the need for new studies to understand this relationship better. Additionally, this investigation may lead to the development of more effective preventive strategies, improving existing treatments and patients’ quality of life.
4. Discussion
The investigation into the effects of daytime sleepiness and sleep-disordered breathing on balance, gait, and the risk of falls revealed significant insights into the relationship between these factors and locomotor health in adults, especially older adults. The two selected articles show a comprehensive view, addressing different aspects of this complex relationship.
4.1. Analysis of the results in the light of the study objectives
This research highlighted the gaps in understanding the relationship between DS and gait/balance and the approach to potentially effective treatments for this population [4, 11]. The case studies and analyses presented illustrate how large-scale randomized controlled trials and investigations are critical to identifying and treating the underlying causes of DS and SDB, preventing its adverse consequences, and determining the efficacy of treatment, consequently promoting greater effectiveness of treatments [10, 11].
4.2. Implications and benefits of daytime sleepiness interventions for gait, balance, and fall prevention
Daytime sleepiness (DS) can impair motor coordination and reaction times [16], affecting the ability to walk steadily and maintain balance. According to Umemura et al. [17], sleep disturbances that generate daytime sleepiness may harm brain areas that could be responsible for the real-time adjustment of gait and sustained attention. This inability increases the risk of falls and compromises mobility and independence [17]. By addressing daytime sleepiness through interventions such as improving sleep hygiene [4, 18], treating sleep disorders, or implementing strategic nap schedules [18, 19], individuals may experience improvements in gait and balance, leading to a reduction in the risk of falls and related injuries [18]. Furthermore, recent research has shown that interventions targeting the root cause of DS, such as cognitive-behavioral therapy for insomnia [20] or personalized pharmacological [13, 21] treatments, have significantly improved balance and motor coordination.
Improved daytime sleepiness and its effects on gait and balance also directly affect fall prevention in seniors and other vulnerable populations [2, 4, 6, 9-11]. Falls are one of the leading causes of injury and hospitalization [10, 12] in the elderly and are often associated with severe consequences such as fractures and functional disability [10, 14]. The risk of fractures is related to the higher likelihood of falls in patients with DS-associated OSA [1, 11] and the adverse effects on motor coordination and balance. When a person is tired, their ability to perceive and react to dangerous situations is reduced, which can lead to falls [22, 23] and, consequently, an increased risk of bone fractures, especially in older people, whose bones tend to be more fragile due to the natural aging process. Studies, such as those conducted by Tyagi et al. [11], have shown that OSA [1, 11] and DS are associated with an increased risk of fall-related fractures, resulting from the difficulty in maintaining vigilance over the adverse effects on motor coordination and balance [17, 22, 23].
In this context, the implementation of targeted interventions can significantly reduce the risk of falls and promote the safety and autonomy of individuals, especially older people.
4.3. Interdisciplinary integration in the management of daytime sleepiness and sleep disorders
The interdisciplinary integration among public health, medicine, dentistry, and others yields significant benefits in treating and researching sleep disorders [2, 6, 10, 12, 14]. Studies, such as those by Lobbezoo et al. [15], indicate that dental sleep medicine traditionally focuses on sleep-related breathing disorders like snoring and obstructive sleep apnea. However, clinical practice reveals that dentistry intersects with other sleep disorders, including sleep-related orofacial pain, xerostomia, hypersalivation, gastroesophageal reflux disease, and bruxism. Recognizing this, a new definition encompassing all aspects of diagnosing and treating these conditions has been formulated for dental sleep medicine.
Moreover, while treatments offer benefits, it’s crucial to consider the challenges associated with DS and SDB-related pathologies and how they can impact treatments [10-13] and, consequently, patient improvement with existing therapeutic interventions. Exploring alternative therapeutic options, such as Integrative and Complementary Practices, may also be significant in treatment and become necessary for various associated pathologies.
In addition, this collaboration can drive innovation in health, such as the development of awareness programs on sleep hygiene, promoting healthy sleep habits from childhood to adulthood. Furthermore, the development of public health policies that promote early detection, as well as the formulation of evidence-based policies aiming to improve access to sleep-related health services and reduce disparities in care provision.
This interconnection among different fields has the potential to positively impact the health of the general population by promoting a culture of healthy sleep and improving healthcare systems as a whole.
4.4. Study limitations
Some limitations of this study merit consideration. Firstly, the methodology employed involved a narrative review of the literature, wherein the examples and case studies presented reflect the research available up to the analysis date without a formal assessment of the included studies' quality. Additionally, it's crucial to note that grey literature was not considered in this review, potentially overlooking valuable insights. Consequently, it’s plausible that recent advancements and applications may not have been addressed in this study.
Moreover, it's worth mentioning that only two articles were analyzed in this narrative review, which inherently restricts the breadth of conclusions drawn. Nevertheless, this caveat does not diminish the topic's significance or the importance of encouraging further research by other scholars.
4.5. Opportunities for research
Future research opportunities encompass longitudinal studies aimed at comprehending the intricate relationship between DS, gait/balance, falls, and associated pathologies, including the risk of trauma such as orofacial fractures. Moreover, investigations should extend to other age groups, mainly focusing on vulnerable populations such as older adults or individuals with underlying medical conditions. This necessitates a meticulous examination of preventive interventions to mitigate risks linked to traffic accidents, encompassing vehicle drivers [17], pedestrians in public areas, machine operators, and school children in both academic and domestic settings.
Given the correlation between DS, fatigue, and other factors compromising cognitive capacity, attention, and risk perception, such research endeavors are pivotal in advancing our understanding and formulating tailored preventive strategies. Furthermore, it's imperative to address the physical, psychosocial, and environmental dimensions, assessing the effectiveness of multidisciplinary interventions involving healthcare, education, and public safety professionals. Notably, the collaboration between health professionals, the community, and research centers, facilitated by their researchers, holds promise in providing valuable insights to enhance the prevention and management of these adverse events, thereby promoting individuals' health and quality of life.
5. Conclusions
This narrative review study highlights the challenge that daytime sleepiness poses to public health, especially among the elderly. It negatively impacts their quality of life and increases the risk of accidents. However, interventions to mitigate daytime sleepiness improve the quality of life of affected individuals and contribute to overall health and well-being, benefiting gait, balance, and fall prevention.
It emphasizes the need to understand the complex interaction between daytime sleepiness, underlying medical conditions, and medication use. When assessing balance, mobility, and the risk of falls, it is essential to consider subjective sleep assessments, as daytime sleepiness can affect cognitive function, attention, reaction time, and motor coordination, thereby increasing the risk of accidents.
While there are no direct studies on the relationship between daytime sleepiness and the risk of orofacial fractures in patients with obstructive sleep apnea, an increase in the likelihood of falls due to daytime sleepiness has been observed. Therefore, there is a need for further direct research on the relationship between sleepiness, fall risk, and fracture risk, filling this knowledge gap and providing more robust insights into the subject.
This study also underscores the importance of interdisciplinary collaboration among healthcare professionals to optimize treatments and develop personalized preventive strategies to reduce the risk of falls in patients with daytime sleepiness.
References
-
W. F. D. Conceição et al., “Obstructive Sleep Apnea Analysis: a literature review,” Revista Eletrônica Acervo Médico, Vol. 20, p. e11247, Nov. 2022, https://doi.org/10.25248/reamed.e11247.2022
-
B. B. Kamdar, K. A. Kaplan, E. J. Kezirian, and W. C. Dement, “The impact of extended sleep on daytime alertness, vigilance, and mood,” Sleep Medicine, Vol. 5, No. 5, pp. 441–448, Sep. 2004, https://doi.org/10.1016/j.sleep.2004.05.003
-
C. Hublin, J. Kaprio, M. Partinen, K. Heikkilä, and M. Koskenvuo, “Daytime sleepiness in an adult, Finnish population,” Journal of Internal Medicine, Vol. 239, No. 5, pp. 417–423, May, 1996, https://doi.org/10.1046/j.1365-2796.1996.475826000.x
-
T. W. Strine and D. P. Chapman, “Associations of frequent sleep insufficiency with health-related quality of life and health behaviors,” Sleep Medicine, Vol. 6, No. 1, pp. 23–27, Jan. 2005, https://doi.org/10.1016/j.sleep.2004.06.003
-
B. Litwiller, L. A. Snyder, W. D. Taylor, and L. M. Steele, “The relationship between sleep and work: A meta-analysis.,” Journal of Applied Psychology, Vol. 102, No. 4, pp. 682–699, Nov. 2016, https://doi.org/10.1037/apl0000169
-
S. Cai, Z. Li, J. Wang, Q. Wang, and R. Chen, “Excessive daytime sleepiness in young and middle-aged Chinese adults with obstructive sleep apnea: implications for cognitive dysfunction,” Sleep and Breathing, Vol. 28, No. 1, pp. 113–121, Jul. 2023, https://doi.org/10.1007/s11325-023-02854-9
-
J. Theorell-Haglöw, T. Åkerstedt, J. Schwarz, and E. Lindberg, “Predictors for development of excessive daytime sleepiness in women: a population-based 10-year follow-up,” Sleep, Vol. 38, No. 12, pp. 1995–2003, Dec. 2015, https://doi.org/10.5665/sleep.5258
-
I. Jaussent, C. M. Morin, H. Ivers, and Y. Dauvilliers, “Incidence, worsening and risk factors of daytime sleepiness in a population-based 5-year longitudinal study,” Scientific Reports, Vol. 7, No. 1, p. 2017, May 2017, https://doi.org/10.1038/s41598-017-01547-0
-
E. Gusman, J. Standlee, K. J. Reid, and L. F. Wolfe, “Work-related sleep disorders: causes and impacts,” Seminars in Respiratory and Critical Care Medicine, Vol. 44, No. 3, pp. 385–395, Apr. 2023, https://doi.org/10.1055/s-0043-1767787
-
S. Tyagi, S. Perera, and J. S. Brach, “Balance and mobility in community‐dwelling older adults: effect of daytime sleepiness,” Journal of the American Geriatrics Society, Vol. 65, No. 5, pp. 1019–1025, Dec. 2016, https://doi.org/10.1111/jgs.14735
-
D. Stevens et al., “The impact of obstructive sleep apnea on balance, gait, and falls risk: a narrative review of the literature,” The Journals of Gerontology: Series A, Vol. 75, No. 12, pp. 2450–2460, Dec. 2020, https://doi.org/10.1093/gerona/glaa014
-
P. Soysal, L. Smith, S. G. Tan, E. Capar, N. Veronese, and L. Yang, “Excessive daytime sleepiness is associated with an increased frequency of falls and sarcopenia,” Experimental Gerontology, Vol. 150, p. 111364, Jul. 2021, https://doi.org/10.1016/j.exger.2021.111364
-
A. C. Reynolds and R. J. Adams, “Treatment of sleep disturbance in older adults,” Journal of Pharmacy Practice and Research, Vol. 49, No. 3, pp. 296–304, May 2019, https://doi.org/10.1002/jppr.1565
-
G. J. Lavigne et al., “Critical issues in dental and medical management of obstructive sleep apnea,” Journal of Dental Research, Vol. 99, No. 1, pp. 26–35, Nov. 2019, https://doi.org/10.1177/0022034519885644
-
F. Lobbezoo, N. de Vries, J. de Lange, and G. Aarab, “A further introduction to dental sleep medicine,” Nature and Science of Sleep, Vol. Volume 12, pp. 1173–1179, Dec. 2020, https://doi.org/10.2147/nss.s276425
-
H. Whittall, M. Pillion, and M. Gradisar, “Daytime sleepiness, driving performance, reaction time and inhibitory control during sleep restriction therapy for Chronic Insomnia Disorder,” Sleep Medicine, Vol. 45, pp. 44–48, May 2018, https://doi.org/10.1016/j.sleep.2017.10.007
-
G. S. Umemura, J. P. Pinho, and A. Forner-Cordero, “Daytime sleepiness affects gait auditory synchronization ability,” in 40th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), pp. 4877–4880, Jul. 2018, https://doi.org/10.1109/embc.2018.8513186
-
J. Redinger, E. Kabil, K. T. Forkin, A. M. Kleiman, and L. K. Dunn, “Resting and recharging: a narrative review of strategies to improve sleep during residency training,” Journal of Graduate Medical Education, Vol. 14, No. 4, pp. 420–430, Aug. 2022, https://doi.org/10.4300/jgme-d-21-01035.1
-
N. S. Redeker, C. C. Caruso, S. D. Hashmi, J. M. Mullington, M. Grandner, and T. I. Morgenthaler, “Workplace interventions to promote sleep health and an alert, healthy workforce,” Journal of Clinical Sleep Medicine, Vol. 15, No. 4, pp. 649–657, Apr. 2019, https://doi.org/10.5664/jcsm.7734
-
P. Cheng, D. Kalmbach, C. Fellman-Couture, J. T. Arnedt, A. Cuamatzi-Castelan, and C. L. Drake, “Risk of excessive sleepiness in sleep restriction therapy and cognitive behavioral therapy for insomnia: a randomized controlled trial,” Journal of Clinical Sleep Medicine, Vol. 16, No. 2, pp. 193–198, Feb. 2020, https://doi.org/10.5664/jcsm.8164
-
P.-Y. Chien, C.-Y. Kuo, M.-H. Lin, Y.-J. Chang, and C.-C. Hung, “Pharmacological interventions for excessive daytime sleepiness in adults with narcolepsy: a systematic review and network meta-analysis,” Journal of Clinical Medicine, Vol. 11, No. 21, p. 6302, Oct. 2022, https://doi.org/10.3390/jcm11216302
-
M. K. Appeadu and B. Bordoni, Falls and Fall Prevention in Older Adults. Treasure Island (FL): StatPearls Publishing, 2024.
-
R. Vaishya and A. Vaish, “Falls in older adults are serious,” Indian Journal of Orthopaedics, Vol. 54, No. 1, pp. 69–74, Jan. 2020, https://doi.org/10.1007/s43465-019-00037-x
About this article
The authors express their gratitude to the Federal University of Minas Gerais (UFMG), the Brazilian National Council for Scientific and Technological Development (CNPQ), and the Coordination for the Improvement of Higher Education Personnel - Brazil (CAPES) – Finance Code 001 for their generous financial support. Additionally, the authors would like to acknowledge the dedicated efforts of the research team in obtaining the results presented in this study.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Wellingtânia Domingos Dias and Junia Maria Serra-Negra worked on the concept and design of the study; Wellingtânia Domingos Dias, also contributed to the management and coordination of the planning and execution of research activities. Additionally, Wellingtânia Domingos Dias, Natalia Espinosa Martínez, Rudolf Huebner and Junia Maria Serra-Negra contributed to the intellectual content of the manuscript, actively participating in the writing of the article and providing critical review and final approval.
The authors declare that they have no conflict of interest.
This article does not contain any studies with human participants performed by any of the authors.
