Abstract
The vertical problems of the stomatognathic system that alter the overbite, either by increasing in the deep bite (DB) or decreasing in the anterior open bite (AOB), are among the great challenges of the dentofacial corrections in the treatment and the retention and stability protocols. It is always good to report that a correct diagnosis is fundamental in the choice of treatment protocol and that skeletal involvement, be it hyper divergence in case of open bite or hypo divergence in case of deep bite, aggravates the problem and as a rule tends to increase treatment and containment time. In this paper the state of art of AOB treatment with Jaw Functional Orthopedics (JFO) will be discussed. It should be emphasized that JFO has a unique diagnostic tool for changes in vertical growth of the face, the Articular Compass, developed by Simões. Studies show that the use of treatment protocols developed by Simões, the SNs (SN2, SN3, SN6) act in the increase of overbite efficiently ( 0.003) in cases of open bite. This is weak evidence, due to the design of the study, but with promising results, so Randomized Clinical Trials are needed to investigate if these results are replicable.
Highlights
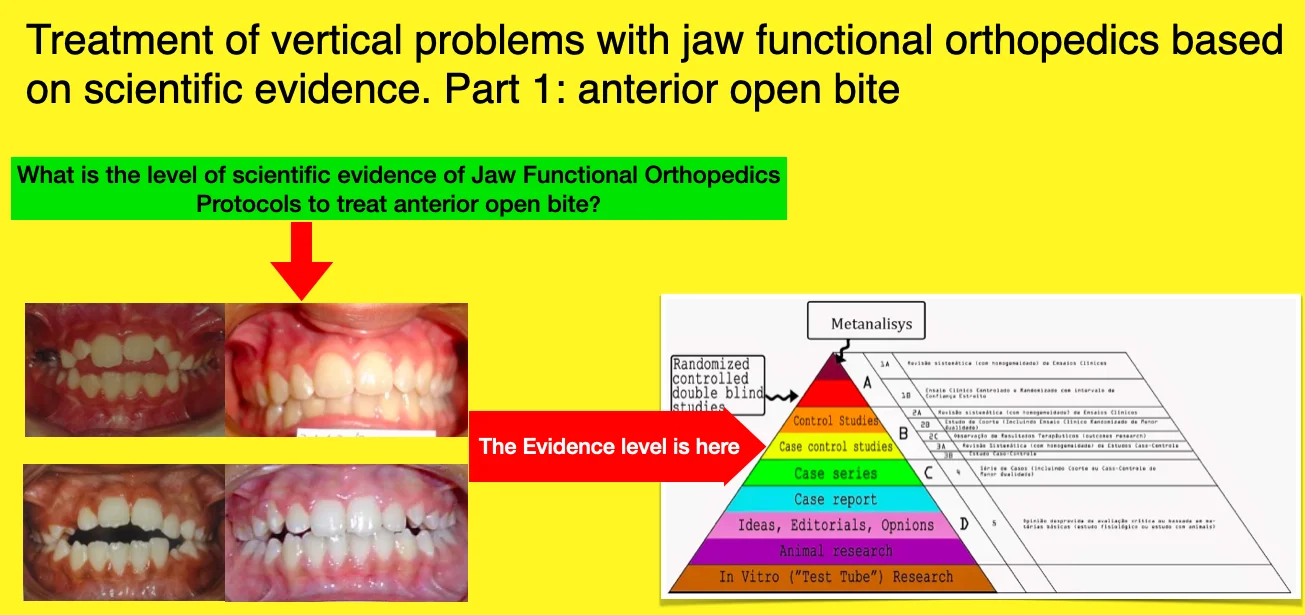
- Evidence suggests that Jaw Functional Orthopedics has protocols to treat anterior open bite.
- The level of evidence of JFO protocols to treat anterior open bite is "case control studies".
- Further studies are necessary to improve evidence level of open bite treatment with JFO.
1. Introduction
Vertical problems, both anterior open bite (AOB) and deep bite (DB), are usually challenging to treat and to retain [1-4]. Craniofacial growth pattern may compromise these malocclusions in a way that only surgical treatment protocol can bring some satisfactory clinical results [5]. Anterior open bite (AOB) retention time and stability are not completely clear [2]. Deep Bite, besides being one of the most common malocclusions has the same status of AOB retention and stability have much to be known [1, 2].
Both malocclusions have a significant impact on orofacial aesthetics and stomatognathic system function and health affecting periodontium, temporomandibular joint (TMJ). Both can change the electrical activity of cervical muscles [6] and can deform cervical vertebrae [5]. Treatment planning of both malocclusions are complex because involve a wide range of factor including psychosocial ones [1-4].
Prevalence of deep overbite was found to be 21 % to 26 % in the normal population [3], and about 75 % in orthodontic patients [7]. The overall prevalence of anterior open bite was 16.52 % in children and adolescents. The prevalence was 19.38 % in South America. The prevalence of anterior open bite was 22.67 % among females and 16.99 % among males. The prevalence of anterior open bite was 18.84 % in the primary dentition, and 14.26 % in the mixed dentition [8]. As can be seen both malocclusions have approximately the same prevalence among general population impacting together from 30 up to 40 % of the general population.
Facial Biotype influence significantly treatment expectations regarding planning, conduction, treatment time, treatment retention and stability [5]. Most of cephalometric analysis have linear and/or angular measurements to study vertical pattern growth of the face as a whole and cranial base, mandibular and maxillary vertical growth pattern separately [9].
Analysis of the divergence growth pattern of the face can bring valuable information to vertical problems treatment. Simões [5, 10] created the Articular Compass cephalometric analysis (Fig. 1) that is an important and crucial tool for vertical problems treatment. An hypodivergent face with a predominance of horizontal growth has a mandibular angle acute and generally a very strong stomatognathic musculature worsening the deep bite treatment prognosis. On the other hand, a hyperdivergent face compromise AOB treatment, sometimes leaving only surgical treatment as an option. The Articular Compass cephalometry also provides information on the degree of impairment of facial growth very useful not only in treatment planning but also on the treatment conduction [5, 10].
Fig. 1Articular Compass cephalometric structural analysis. Figure Extracted from Simões [10]
![Articular Compass cephalometric structural analysis. Figure Extracted from Simões [10]](https://static-01.extrica.com/articles/22778/22778-img1.jpg)
Fig. 2Divergent occlusal plane – Plane/Plane. Figure extracted from Simões [5]
![Divergent occlusal plane – Plane/Plane. Figure extracted from Simões [5]](https://static-01.extrica.com/articles/22778/22778-img2.jpg)
Fig. 3Divergent occlusal plane – Curve/Plane

Analysis of the pathology of the occlusal plane is also a very important data and has to be considered in both malocclusion treatment. In AOB, a divergent occlusal plane classified as plane/plane (Fig. 2) were there is no curve on the occlusal plane and usually with occlusal contacts on in the last teeth of the arch worsen AOB treatment prognosis while the divergent occlusal plane classified as curve/plane (Fig. 3) improves prognosis. There must be treatment protocol differences between both situations, on the first mandibular rotation is needed, on the second, sometimes only anterior teeth movement is necessary for the AOB correction.
2. Anterior open bite treatment scientific evidence
There are several treatment protocols for AOB with the efficiency scientifically proved such as mini-implants (mini screws of mini plates) [11, 12], aligners [13-15], headgear [16], posterior build ups [17], surgical treatment [18], bite blocks [19] among others.
In a systematic review, Santos et al [20] reported that there was insufficient evidence to allow inference to be drawn about the effects of AOB treatment with the functional orthopedic appliances used in the treatment. In the Randomized Clinical Trials (RCT), they identified, and recovered the techniques used by Fränkel, a comparison between fixed and removable palatal crib, chin cap and bonded spurs. They included any type of functional appliance used for AOB treatment such as Fränkel, Bionator, Sns, Bimler, Planas in comparison with a no treatment, alternative treatment or wait-list control.
Soares and Santiago [21] in a retrospective study in a sample with a wide range age reported efficiency of Jaw Functional Orthopedics in the treatment of AOB (P = 0,003). Even though, there is still little evidence of the efficiency of Jaw Functional Orthopedics in AOB treatment. Soares and Santiago [20] findings are promising but the strength of the data is weak based on the scientific evidence pyramid.
In their paper, Santos et al. [20] did not separate mechanical orthopedics and functional orthopedics. They found papers where the only functional orthopedic technique used was the Fränkel technique, the other types (crib, chin cup, and bonded spurs) are mechanical orthopedics appliances denoting the scarcity of investigation with functional orthopedics appliances. Their conclusion that high quality RCTs are needed reveals the necessity of investigations of clinical results and modus operandi of functional orthopedics appliances.
The mechanism of action of JFO in the treatment of anterior open bite is still unknown taking into consideration scientific evidence. With mechanical orthopedics, rotation of mandible and maxilla is already proved [13, 16, 19]. There are some theories about how JFO modifies the stomatognathic system but none proved. Costa et al [22] found a weak correlation of the mandibular degree of closure ( 0,098). No other paper regarding this subject was found in Capes Portal or Medline using key words “anterior open bite”, “treatment”, “skeletal changes”, “mechanism”, “dentofacial orthopedics”, “jaw functional orthopedics” and “functional orthopedics”.
3. Conclusions
There are weak evidences that JFO is effective in AOB treatment.
Randomized Clinical Trials are needed for a profounder view in this subject.
References
-
M. M. El Namrawy, F. El Sharaby, and M. Bushnak, “Intrusive arch versus miniscrew-supported intrusion for deep bite correction,” Open Access Macedonian Journal of Medical Sciences, Vol. 7, No. 11, pp. 1841–1846, Jun. 2019, https://doi.org/10.3889/oamjms.2019.332
-
A. A. Gianelly, J. C. Petras, and J. Boffa, “Condylar position and Class and Class II deep-bite, no-overjet malocclusions,” American Journal of Orthodontics and Dentofacial Orthopedics, Vol. 96, No. 5, pp. 428–432, Nov. 1989, https://doi.org/10.1016/0889-5406(89)90328-4
-
C. Rijpstra and J. A. Lisson, “Etiology of anterior open bite: a review,” Journal of Orofacial Orthopedics / Fortschritte der Kieferorthopädie, Vol. 77, No. 4, pp. 281–286, Jul. 2016, https://doi.org/10.1007/s00056-016-0029-1
-
L. S. Todoki et al., “The national dental practice-based research network adult anterior open bite study: treatment success,” American Journal of Orthodontics and Dentofacial Orthopedics, Vol. 158, No. 6, pp. e137–e150, Dec. 2020, https://doi.org/10.1016/j.ajodo.2020.07.033
-
W. A. Simões, Ortopedia Funzionale dei Mascellari Atraverso la Riabilitazione Neuro-Oclusale. (in Italian), Orbetello, 2010.
-
R. Miralles et al., “Vertical dimension. Part 2: the changes in electrical activity of the cervical muscles upon varying the vertical dimension,” CRANIO®, Vol. 20, No. 1, pp. 39–47, Jan. 2002, https://doi.org/10.1080/08869634.2002.11746189
-
W. Proffit, H. J. Fields, and L. J. Moray, “Prevalence of malocclusion and orthodontic treatment need in the US,” International Journal of Adult Orthodontics and Orthognathic Surgery, Vol. 13, pp. 97–106, 1998.
-
M. T. Avrella, D. R. Zimmermann, J. S. P. Andriani, P. S. Santos, and J. C. Barasuol, “Prevalence of anterior open bite in children and adolescents: a systematic review and meta-analysis,” European Archives of Paediatric Dentistry, Vol. 23, No. 3, pp. 355–364, Jun. 2022, https://doi.org/10.1007/s40368-021-00683-6
-
F. J. Aguila, Manual de Cefalometría.1st Ed. Actualidades Médico Odontológicas Latinoamericana. (in Spanish), Caracas, 1996.
-
W. A. Simões, “Articular Compass: The Location of Frontal Accessories of Bioelastic Appliances,” CRANIO®, Vol. 17, No. 2, pp. 109–125, Apr. 1999, https://doi.org/10.1080/08869634.1999.11746085
-
H. E. Kassem and E. S. Marzouk, “Prediction of changes due to mandibular autorotation following miniplate-anchored intrusion of maxillary posterior teeth in open bite cases,” Progress in Orthodontics, Vol. 19, No. 1, pp. 1–7, Dec. 2018, https://doi.org/10.1186/s40510-018-0213-5
-
A. Cambiano, G. Janson, D. Lorenzoni, D. Garib, and D. Dávalos, “Nonsurgical treatment and stability of an adult with a severe anterior open-bite malocclusion,” Journal of Orthodontic Science, Vol. 7, No. 1, 2018, https://doi.org/10.4103/jos.jos_69_17
-
S. Moshiri, E. A. Araújo, J. F. Mccray, G. Thiesen, and K. B. Kim, “Cephalometric evaluation of adult anterior open bite non-extraction treatment with Invisalign,” Dental Press Journal of Orthodontics, Vol. 22, No. 5, pp. 30–38, Oct. 2017, https://doi.org/10.1590/2177-6709.22.5.030-038.oar
-
R. Khosravi et al., “Management of overbite with the Invisalign appliance,” American Journal of Orthodontics and Dentofacial Orthopedics, Vol. 151, No. 4, pp. 691–699.e2, Apr. 2017, https://doi.org/10.1016/j.ajodo.2016.09.022
-
K. Harris et al., “Evaluation of open bite closure using clear aligners: a retrospective study,” Progress in Orthodontics, Vol. 21, No. 1, pp. 1–9, Dec. 2020, https://doi.org/10.1186/s40510-020-00325-5
-
S. Sambataro et al., “Cephalometric changes in growing patients with increased vertical dimension treated with cervical headgear,” Journal of Orofacial Orthopedics / Fortschritte der Kieferorthopädie, Vol. 78, No. 4, pp. 312–320, Jul. 2017, https://doi.org/10.1007/s00056-017-0087-z
-
A. Vela-Hernández, R. López-García, V. García-Sanz, V. Paredes-Gallardo, and F. Lasagabaster-Latorre, “Nonsurgical treatment of skeletal anterior open bite in adult patients: Posterior build-ups,” The Angle Orthodontist, Vol. 87, No. 1, pp. 33–40, Jan. 2017, https://doi.org/10.2319/030316-188.1
-
M. Wang, B. Zhang, L. Li, M. Zhai, Z. Wang, and F. Wei, “Vertical stability of different orthognathic treatments for correcting skeletal anterior open bite: a systematic review and meta-analysis,” European Journal of Orthodontics, Vol. 44, No. 1, pp. 1–10, Jan. 2022, https://doi.org/10.1093/ejo/cjab011
-
V. Paoloni, D. Fusaroli, L. Marino, M. Mucedero, and P. Cozza, “Palatal vault morphometric analysis of the effects of two early orthodontic treatments in anterior open bite growing subjects: a controlled clinical study,” BMC Oral Health, Vol. 21, No. 1, pp. 1–9, Dec. 2021, https://doi.org/10.1186/s12903-021-01886-5
-
E. Marcílio Santos et al., “Functional orthopedic treatment for anterior open bite in children. A systematic review of randomized clinical trials,” Journal of Orofacial Orthopedics / Fortschritte der Kieferorthopädie, pp. 1–10, Apr. 2022, https://doi.org/10.1007/s00056-022-00388-5
-
E. Teixeira Costa, I. Piramo Moreira Santiago, and O. Santiago Júnior, “Study of skeletal changes in individuals with anterior open bite treated with JFO,” Jaw Functional Orthopedics and Craniofacial Growth, Vol. 2, No. 1, pp. 16–21, Jun. 2022, https://doi.org/10.21595/jfocg.2022.22723
-
M. T. C. Soares and O. Santiago, “Is jaw functional orthopedics an efficient tool to treat anterior open bite? A retrospective study,” Jaw Functional Orthopedics and Craniofacial Growth, Vol. 2, pp. 11–15, Jun. 2022, https://doi.org/10.21595/jfocg.2022.22682
About this article
The authors have not disclosed any funding.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
