Abstract
Functional Orthopedics appliances must follow strict rules of construction and respect the correct indications, to achieve the proposed goals. The approach must be individualized for each patient according to each needing. Dr Wilma Alexandre Simões created a network of appliances, with no similarity with other appliances created by other authors. Her appliances respect rigid scientific fundamentals and provide for the clinician special tools for solving different types of occlusopathies. Here we present some rules, developed, and scientifically supported by the authors, in order to optimize the use of one of Simões Network called SN2.
Highlights
- Simões Network 2 (SN2) is an amazing bioelastic appliance used to change tongue posture.
- The main excitation point of SN2 is the tip of the tongue due to high density of sensorial receptors.
- The confection of SN2 must follows rigid rules, otherwise the objective will not be completely achieved.
- The anterior inferior notch confection is guided by expected therapeutic posture changing.
1. Introduction
The tongue has a high level of mechanosensitivity. Particularly, the tip of the tongue can be compared to the fingertip in terms of sensitivity, expressing an extremely detailed acuity [1, 2]. On Penfield Homunculus we can realize the huge importance of tongue with a big representation on somatosensory cortex [3]. Few studies have drawn the attention to the importance of tongue tip afferences for the correct tongue motor efferences [4]. However, recently, a wonderful review defined the tongue regions related to somatosensory inputs [5] and a study using electrostimulation in anesthetized humans showed the big interaction between trigeminal afferences and Hypoglossal efferences [6] Together these studies support the clinical observation that tongue is able to sense the accessories placed in an appliance and generate the motor efferences that will lead to tongue and mandible posture changing. When posture is changed, automatically, by bone mechanotransduction mechanisms, we have a different pattern of bone remodeling [7]. Based on the peculiarity of oral cavity sensitivity, Dr Wilma Simões developed a sequence of appliances called Simões Network. The objective of this work is to present some extremely important physiologic details that must guide the confection of one of these appliances, called SN2 [8] Fig. 1.
2. Clinical relevance
Tongue posture alteration is an important etiologic factor of occlusopathies. SN2 was designed to stimulate specific regions of the tongue and generate alteration on tongue posture inside the mouth, leading to the correction of these occlusopathies.
2.1. Indications
Simões described 21 indications for SN2 [8], all of them related to the possibility of guiding the tongue to its correct position inside the mouth, leading to mandible posture changing in sagittal, lateral, and vertical direction. SN2 is an extremely versatile appliance, occupying very little oral space.
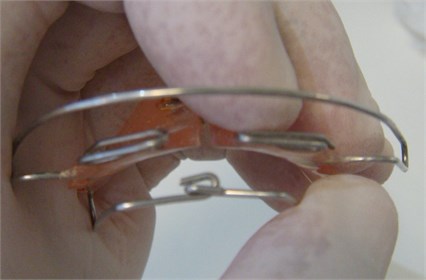
Fig. 1Close view of the SN2 dorsal arch. The bending of the wire to make the notch must be just a fold and the connection of vertical and horizontal bending cannot be tightened, to allow small lateral movements
2.2. Mechanism of action
The specific design of the dorsal arch, creating a notch on the midline, generate different type of sensitive stimuli. Since many decades it was known that the anterior region of the tongue has different receptive fields with a huge density of receptors. However, recent studies in humans showed perfectly how the touch on different regions elicit different muscle activity [9-11]. The sagittal part of the dorsal arch touches on the tongue lateral side and the anterior notch touches on the tongue tip, generating activation of styloglossus (as main muscle, considering that all tongue and related muscles will be also activated), having, as a result, tongue transversal size diminishing, dorsal elevation, and up-down movement of the tip [12-14]. Considering this high level of tongue sensitivity, the construction of the appliance must follow rigid rules that cannot be despised.
2.3. Construction details
The main component of SN2 is the dorsal arch described on Fig. 1. The connection between right and left make a notch that has important construction rules. It is made by 2 simple bands of the wire, one horizontal and one vertical. When they connect each other, they cannot be tightened, since we need some movement of this assembly following mandible/tongue movements Fig. 1. We must always remember that SN2 is a very bioelastic appliance with huge flexibility.
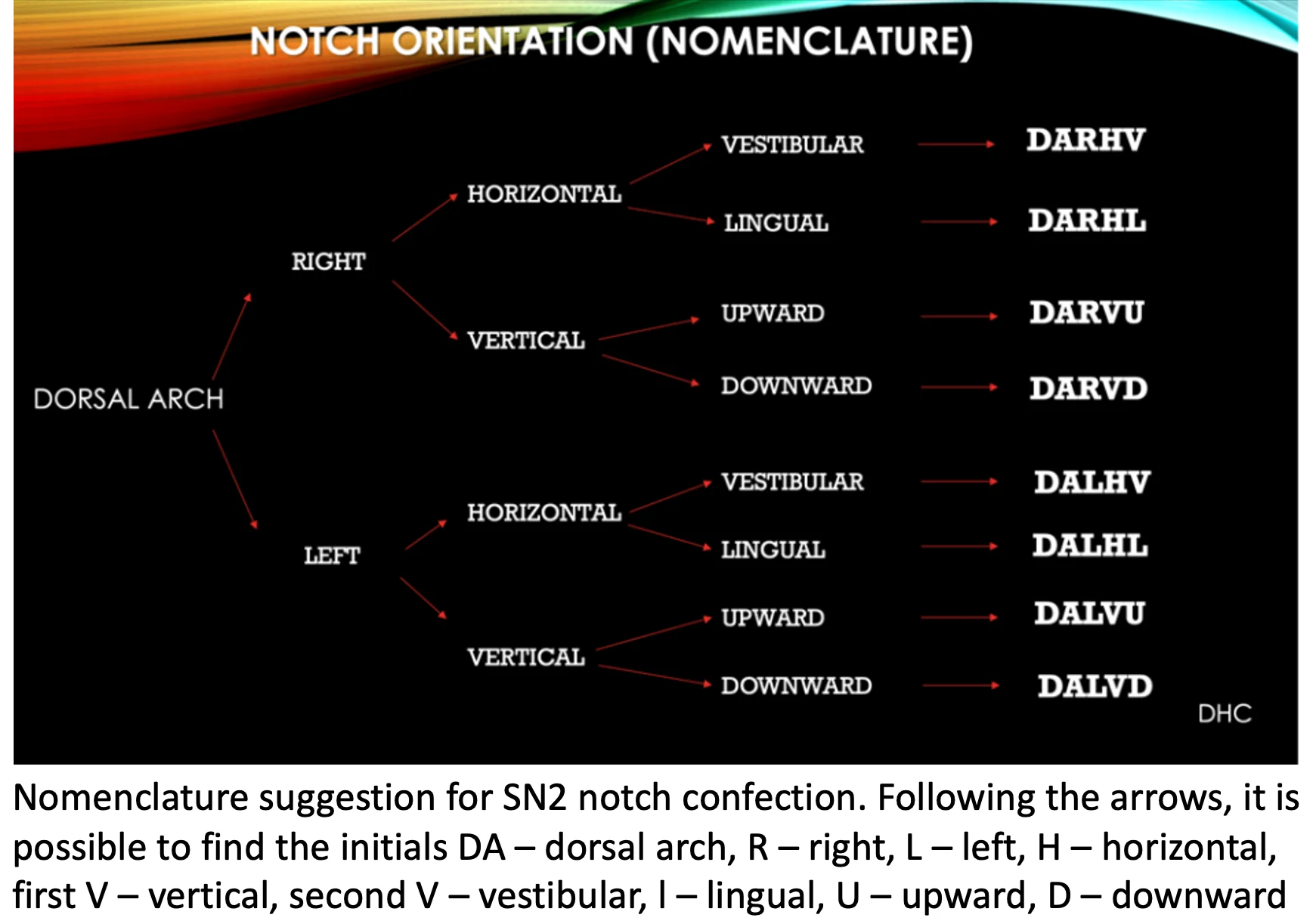
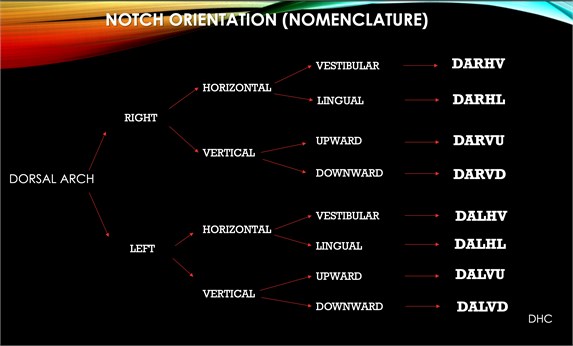
The lateral part of dorsal arch must come straight from posterior entrance into superior acrylic, until the edge between canine and lateral incisor. The anterior part, that will generate the notch, must also be straight. There is no curvature on the wire arms. The orientation of the notch bending will depend on the purpose of the clinician. The technician is not able to define this, since the tongue position alteration observed on clinical exam will determine the direction of the bending. The final part of the wire can be showing up to the tongue or ridded on the direction of the teeth (showing to vestibular side). So, the horizontal notch can send the tongue tip up or down and the vertical tongue can send the tongue to right or left. When the end of the wire is hidden the main effect will be elevation of tongue dorsal region and diminishing of transversal dimension. It is necessary to explain exactly to the technician the appliance receipt. On Fig. 2 there is a suggestion of nomenclature to be used for clinician/technician communication.
It is important to reinforce that the traditional superior part of the SN2 is made by a palatal acrylic plate with frontal accessories and screw, designed and placed according to each case and following WAS specifications [8]. The appliance does not have clamps. It must be free in the mouth to achieve the goals.
Fig. 2Nomenclature suggestion for SN2 notch confection. Following the arrows, it is possible to find the initials DA – dorsal arch, R – right, L – left, H – horizontal, first V – vertical, second V – vestibular, l – lingual, U – upward, D – downward
3. Discussion
Tongue is a complex part of the stomatognathic system and is innervated by 5 different cranial nerves having a sophisticated sensorimotor performance on mouth functions. The muscles involved on tongue function are not only the intrinsic and extrinsic tongue muscles, but also the supra and infrahyoid muscles, as well as all the muscles and ligaments connected to hyoid bone. Hyoid is the support of the tongue and is the only bone in the body that does not have direct connection with other bones [15]. Due to that, when we change the biomechanics of the tongue, we also change afferences, efferences and remodeling stimuli in different sites of the system [16]. The spatial configuration of tongue assembly is extremely sensitive to little touches and a single stimulus generates answer in all muscles from this complex system [17, 18]. Taking all this knowledge in consideration, Dr. Wilma Simões designed the SN2 with a very light configuration but amazing effect.
4. Conclusions
SN2 is a very useful functional appliance that has a great number of indications and provides adequate bone remodeling when manufactured according to rigid rules.
References
-
B. L. Miles, K. van Simaeys, M. Whitecotton, and C. T. Simons, “Comparative tactile sensitivity of the fingertip and apical tongue using complex and pure tactile tasks,” Physiology and Behavior, Vol. 194, pp. 515–521, Oct. 2018, https://doi.org/10.1016/j.physbeh.2018.07.002
-
R. W. van Boven and K. O. Johnson, “The limit of tactile spatial resolution in humans: Grating orientation discrimination at the lip, tongue, and finger,” Neurology, Vol. 44, No. 12, pp. 2361–2361, Dec. 1994, https://doi.org/10.1212/wnl.44.12.2361
-
F.-E. Roux, I. Djidjeli, and J.-B. Durand, “Functional architecture of the somatosensory homunculus detected by electrostimulation,” The Journal of Physiology, Vol. 596, No. 5, pp. 941–956, Mar. 2018, https://doi.org/10.1113/jp275243
-
J.-F. Patri, J. Diard, and P. Perrier, “Modeling sensory preference in speech motor planning: a Bayesian modeling framework,” Frontiers in Psychology, Vol. 10, Oct. 2019, https://doi.org/10.3389/fpsyg.2019.02339
-
Y. Moayedi, S. Michlig, M. Park, A. Koch, and E. A. Lumpkin, “Somatosensory innervation of healthy human oral tissues,” Journal of Comparative Neurology, Vol. 529, No. 11, pp. 3046–3061, Aug. 2021, https://doi.org/10.1002/cne.25148
-
A. Szelényi and E. Fava, “Long latency responses in tongue muscle elicited by various stimulation sites in anesthetized humans – new insights into tongue-related brainstem reflexes,” Brain Stimulation, Vol. 15, No. 3, pp. 566–575, May 2022, https://doi.org/10.1016/j.brs.2022.03.003
-
M. Herrmann et al., “Interactions between muscle and bone-where physics meets biology,” Biomolecules, Vol. 10, No. 3, p. 432, Mar. 2020, https://doi.org/10.3390/biom10030432
-
Simões W. A., Ortopedia Funzionale dei Mascellari. Attraverso la Riabilitazione Neuro – Oclusale. 2010.
-
H. Maezawa et al., “Functional cortical localization of tongue movements using corticokinematic coherence with a deep learning-assisted motion capture system,” Scientific Reports, Vol. 12, No. 1, pp. 1–11, Dec. 2022, https://doi.org/10.1038/s41598-021-04469-0
-
H. Maezawa, “Cortical mechanisms of tongue sensorimotor functions in humans: a review of the magnetoencephalography approach,” Frontiers in Human Neuroscience, Vol. 11, Mar. 2017, https://doi.org/10.3389/fnhum.2017.00134
-
A. Schippers, M. J. Vansteensel, Z. V. Freudenburg, F. S. S. Leijten, and N. F. Ramsey, “Detailed somatotopy of tongue movement in the human sensorimotor cortex: A case study,” Brain Stimulation, Vol. 14, No. 2, pp. 287–289, Mar. 2021, https://doi.org/10.1016/j.brs.2021.01.010
-
Sarah Akbar and Marc H. Hohman, “Anatomy, Head and Neck, Styloglossus,” StatPearls Publishing, Sep. 2021.
-
Y. Sakamoto, “Morphological features of the branching pattern of the hypoglossal nerve,” The Anatomical Record, Vol. 302, No. 4, pp. 558–567, Apr. 2019, https://doi.org/10.1002/ar.23819
-
A. Mirallave Pescador et al., “Methodology for eliciting the brainstem trigeminal-hypoglossal reflex in humans under general anesthesia,” Clinical Neurophysiology, Vol. 137, pp. 1–10, May 2022, https://doi.org/10.1016/j.clinph.2022.02.004
-
G. Messina, “The tongue, mandible, hyoid system,” European Journal of Translational Myology, Vol. 27, No. 1, Mar. 2017, https://doi.org/10.4081/ejtm.2017.6363
-
Y. Kajee, J.-P. V. Pelteret, and B. D. Reddy, “The biomechanics of the human tongue,” International Journal for Numerical Methods in Biomedical Engineering, Vol. 29, No. 4, pp. 492–514, Apr. 2013, https://doi.org/10.1002/cnm.2531
-
Y. Sakamoto, “Configuration of the extrinsic muscles of the tongue and their spatial interrelationships,” Surgical and Radiologic Anatomy, Vol. 39, No. 5, pp. 497–506, May 2017, https://doi.org/10.1007/s00276-016-1777-8
-
I. Sanders and L. Mu, “A three-dimensional atlas of human tongue muscles,” The Anatomical Record, Vol. 296, No. 7, pp. 1102–1114, Jul. 2013, https://doi.org/10.1002/ar.22711

