Abstract
The maintenance of the lower level of muscle contraction is fundamental for the development and health of the stomatognathic system (SS). Malocclusion leads to unbalance muscle activity, since Class II treatment is not the most prevalent malocclusion in the general population but is the more frequent to search for treatment in dental offices and the most prevalent skeletal component in the class II malocclusion is the retrognathia this pilot investigation aims to study the effect of rest electric activity of bilateral anterior temporal, masseter and suprahyoid muscle in individuals undergoing class II treatment with functional orthopedic appliance Simões Network 6 (SN6). Surface electromyography recordings of bilateral anterior temporal, masseter and suprahyoid muscle in rest position was obtained before and 8 minutes after the functional appliance insertion in mouth. Results showed improvement of electric muscle activity in rest position and balance of bilateral muscle electric activity in all muscle. Based on the preliminary results it can be conclude that jaw functional orthopedics (JFO) provides alteration of the resting records in the mandibular rest position of the studied muscles, indicating relaxation of the muscles studied and a more symmetrical electric activity. Further studies are necessary for a better understanding of the effects of functional orthopedic appliances in the electric activity of stomatognathic muscle in the mandibular rest position.
Highlights
- Balance muscle activity in class II treatment with SN6- sEMG recording
- Lowering rest mandibular position muscle tone with functional orthopedic appliance during Class II treatment
- Use of sEMG in jaw functional orthopedics
- Use of sEMG in Dentistry
1. Introduction
Balance of stomatognathic muscle is fundamental for the development and health of the stomatognathic system (SS) both in function and in rest. Unbalance of these muscle in malocclusion or clenching/grinding (bruxism), for instance, tends to bring harmful consequences for structures of the SS like maxillary bones, muscle, temporomandibular joint (TMJ), periodontium, dental structures etc., due to pathological mechanical request of the entire system. [1, 2].
Class II treatment is not the most prevalent malocclusion in the general population but is the more frequent to search for treatment in dental offices [3]. For more than 40 years is know that the most prevalent skeletal component in the class II malocclusion is the retrognathia [4], for such, the most indicated treatment protocol for Class II is the mandibular protrusion, called from now on as mandibular advancement. This mandibular advancement can be achieved with mechanical orthopedic appliances (appliances attached permanently in the mouth) as Herbst appliance, orthognathic surgery [5] and FOA in children [6] and adults [7].
Bogdanov et al. [6] reported and improvement of children with class II division 1 malocclusion after the use of functional orthopedic appliance (FOA) trainer T4K. The authors show improvement of anterior temporal and masseter muscle contraction pattern during clenching. Xia et al. [8] reported that the class II division 1 treatment with twin block appliance increase the maximum voltage and asymmetry index of anterior temporalis and masseter muscle.
Simões [9] stablished that when the individual in treatment with Jaw Functional Orthopedics (JFO) touches the buccal incisal third of the inferior incisor with the lingual incisal third of the superior incisor – touch in DA with the FOA the supreme stimulation of the SS is achieved and the individual being able to keep the touch in DA without the appliance is a land mark and SS has a better muscular balance. Sakai et al. [10] reported that during treatment with (JFO) when the individuals are able to maintain the touch in DA without the FOA in mouth were found a bilateral equilibrium of surface electromyography (sEMG) registration of the anterior temporal and masseter muscle, due to a homogenization of bilateral muscle, were found a diminishing the sEMG registration in Amplitude, Pattern Deviation and Media, in all situation and moments.
The peri oral muscle like orbicularis oris and mentalis are compromised too in Class II division 1 individuals [7], Bogdanov et al. reported improvement in the orbicularis oris function after class II correction with JFO.
The aim of the present investigation is a pilot study to observe the behavior of the electrical activity of bilateral masseter, anterior temporal, and suprahyoid muscle in the mandibular rest position measured by sEMG immediately after insertion of an Simões Network 6 (SN6) [9] FOA for mandibular advancement in a class II division 1 malocclusion.
2. Methodology
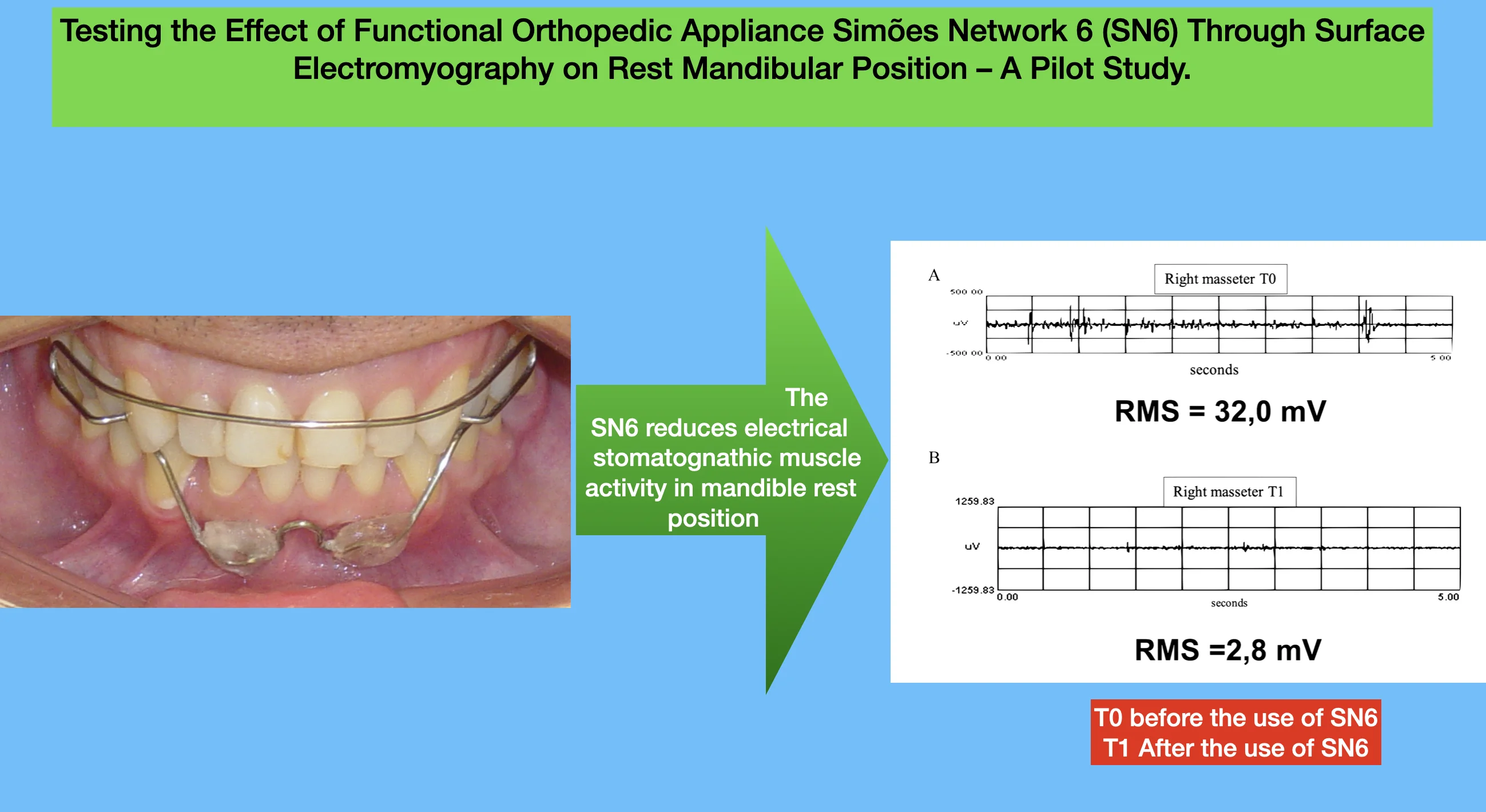
After a complete clinical examination, gnatostathic and radiographic diagnosis a 14 years old boy was diagnosed with Class II division 1 malocclusion. Poor oral health, no tooth decay, all posterior teeth except tooth 14 with amalgam restorations, teeth 11, 12, 21, 22 with resins and, as can see in Fig. 1 plaque in the cervical region of 43, 31, 32, 33. Due to a vertical biotype the FOA prescribed was an SN6 due to its capacity to create an instant axis of rotation. In Figure 1, in the upper image the buccal arch can be seen in the maxilla. I the mandible the descent of the dorsal arch to hold the special shields and the inverted “V” that join the left and right special shields. The special shields are made in acrylic and its superior part can also be seen. In the middle image patient with the mouth opened the inferior part of the appliance can be seen. It is composed by the dorsal arches, a wavy bar, the inferior winglets that joins the dorsal arches to the wavy bar. It is always good to remember that it is not a lingual grid, the aim of the wavy bar is to educate the tongue not to hold the tongue, for such it has very specific geometry, frontiers and positions that can be seen in Simões [9]. In the inferior image of figure 1 it can be seen the relationship of the special shield with the patient mucosa, it is very close but do not touch the mucosa, there is no ischemic area in the mucosa.
Use sEMG is based on fact that this is a technology in growing use around the world, in different Research Centers, with more and more comprovation as a good methodology and results,the large experience in use it by our researchers; the possible opportunity to collaborate to better recognition by scientific community by use sEMG was very attractive too. sEMG data was collected with the individual sat in an upright position, Camper Plan parallel to the ground, without head support, sole of the foot touching the ground in its entirety, tights parallel to the ground, hands resting on thighs. sEMG recordings were made of bilateral anterior temporal, masseter and suprahyoid muscle. All collections were performed in a controlled environment (ambient temperature, noise, humidity, lighting, isolation in relation to direct electoral current (no source of direct current in the laboratory environment was active, including all sources of electrical energy used were batteries); all collections, at all times and situations were done bilaterally. Electromyograph EMG1000, from Lynx Electronics – Brazil; bipolar electrodes, with a standardized distance of 2 centimeters; earth electrode Made in Canada; we did not make use of normalization of EMG signals. sEMG recordings were made in T0 (in the diagnosis session) and T1 (8 minutes after the installation of the SN6 on the patient’s mouth) based on the methodology used by Sakai et al. [10]. This study was approved by the Ethic committee of State University of Campinas (Piracicaba, Brazil) UNICAMP under protocol 159/2004.
Fig. 1SN6 installed in patient’s mouth. In the upper image the buccal arch can be seen in the maxilla. I the mandible the descent of the dorsal arch to hold the special shields and the inverted “V” that join the left and right special shields. The special shields are made in acrylic and its superior part can also be seen. In the middle image patient



3. Results
In Fig. 2 can be observed the sEMG registration in T0 with the Root mean square (RMS) of left temporal. It can be observed that the RMS in T0 was 32,0 mV and in T1 was 4.4 mV. The sharp decrease of left anterior temporal can be observed with electric activity of the muscle much closer to zero. On the recordings of right anterior temporal muscle (Fig. 3) the RMS remained the same but much closer in T1 of the left anterior temporal recordings of the left side in (T1 RMS of left temporal is 4,4 mV and right temporal is 3,7 mV showing more symmetry in electric activity of bilateral anterior temporal muscle in rest position in T1.
Fig. 2sEMG recordings of left temporal muscle: a) sEMG recordings in T0 of left anterior temporal muscle in T0 with RMS, b) recordings in T1 of left anterior temporal muscle with RMS in yellow
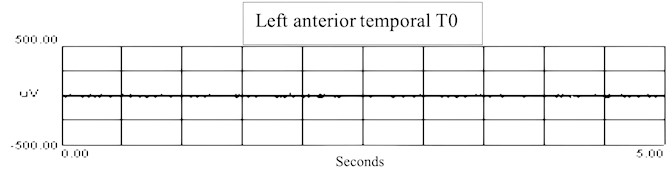
a) RMS = 32.0 mV
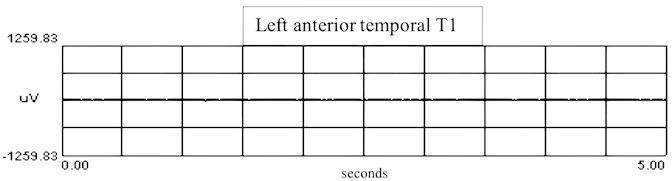
b) RMS = 4.4 mV
Fig. 3sEMG recordings of right temporal muscle: a) sEMG recordings in T0 of right anterior temporal muscle in T0 with RMS, b) recordings in T1 of right anterior temporal muscle with RMS
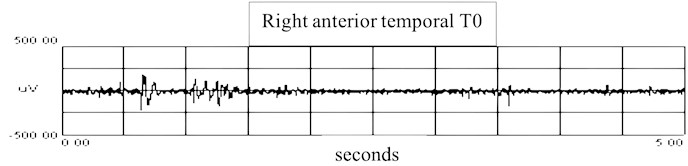
a) RMS = 3.1 mV
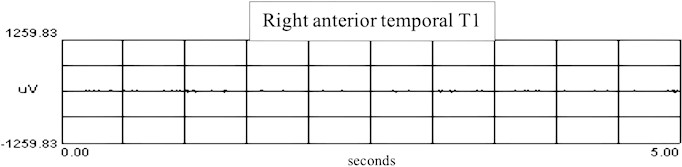
b) RMS = 3.7 mV
Fig. 4sEMG recordings of left masseter muscle: a) sEMG recordings in T0 of left masseter muscle in T0 with RMS, b) recordings in T1 of left masseter muscle with RMS
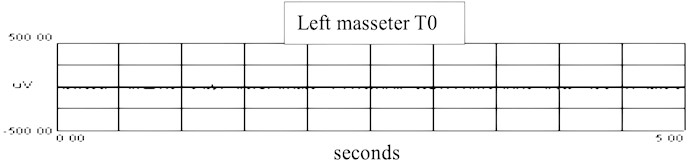
a) RMS = 19.4 mV
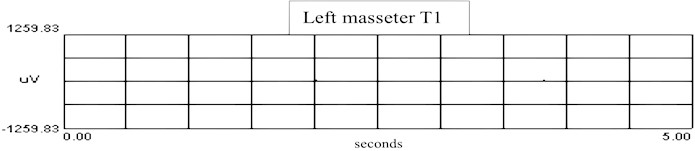
b) RMS = 14.1 mV
Fig. 5sEMG recordings of right masseter muscle: a) sEMG recordings in T0 of right masseter muscle in T0 with RMS, b) recordings in T1 of right masseter muscle with RMS
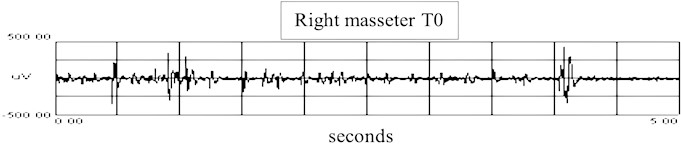
a) RMS = 32.9 mV
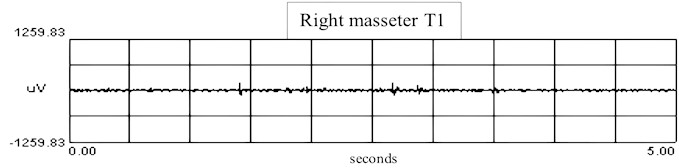
b) RMS = 2.8 mV
In Fig. 4 recordings of left masseter muscle can be observed in T0 and T1. The RMS diminish from 19,4 mV to 14,1 mV a much less pronounced decrease the one observed on both sides of the anterior temporal muscle in Fig. 1. On the other hand, the right side masseter (Fig. 5) followed the behavior of the anterior temporal muscle and had a RMS decrease from 32,0 mV to 2,8 mV.
The recordings of the suprahyoid muscle (Fig. 6) did not show a considerable change with the same behavior of the right anterior temporal muscle (Fig. 3). In T1 the RMS of all studied muscle but the left masseter showed similar values, around 3 and 4 mV.
Fig. 6sEMG recordings of suprahyoid muscle: a) sEMG recordings in T0 of suprahyoid muscle in T0 with RMS, b) recordings in T1 of suprahyoid muscle with RMS
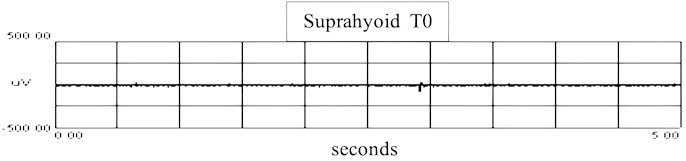
a) RMS = 3.1 mv
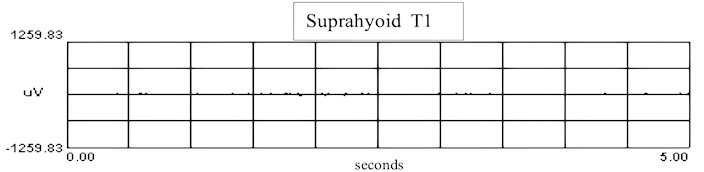
b) RMS = 4.2 mv
4. Discussion
The results found showed that the RMS electric activity in T0 bilaeral temporal muscle, right masseter and suprahioyd muscle are far from zero, and the left masseter was close to zero. In T1 they were closer to zero in bilateral temporal muscle, bilateral masseter, suprahioyd muscle, showing change in the RMS all studied muscle except the right masseter due to its RMS was already close to zero in T0. It seems that a balance of the musculature was achieved with a more symmetrical electric activity of the studied muslce. The decrease on the sEMG activity in rest position found in this pilot study, with all the limitations inherent of the sample and design of a pilot study, is in accordance to Santiago et al. [11] DTM study that shows decrease in muscle, articular and neck pain in individuals with TMD treated with Jaw Functional Orthopedics (JFO) of course, further investigations are needed to comprehend and check the analogy. Bogdanov et al. [6] reported improvement of muscle condition after class II treatment with FOA, both studies results suggest that JFO maybe a tool to treat some chronic pain TMD patients with non-conservative treatment.
Investigations with different types of appliances [5, 6] advancing the mandible in class II treatment with retrognathia improved que maximum contractile of masseter and anterior temporal muscle denoting more muscle capacity to crunch the food, improving masticatory efficiency in the treated individuals. This pilot study suggests that the electric activity of stomatognathic muscle is improved in rest position too, suggesting a full SS rehabilitation with JFO improving occlusion, and muscle balance in function and rest, associated to a better self-esteem.
The findings are in accordance with Sakai et al. [10] which reported that during treatment with JFO the electric activity of stomatognathic muscle is improved. On the other hand, the construction of the functional orthopedic appliance seems to be checked with sEMG as propose Santiago et al in other study testing SN10 appliance.
This is just a pilot study, but the results show a decreasing and symmetric electric activity of stomatognathic muscle when functional orthopedic appliance – SN6 is in mouth. Although Julious [12] proposed a sample size of 12 per group for pilot studies based on feasibility, precision about the mean and variance, and regulatory considerations there are so many variables that we are dealing with (there would be an electromyographic change with placement of the appliance in mouth? How long after placement of the appliance in mouth there would be an electromyographic change? Was T1 a good interval? and so on) that we decide to publish the initial data to show the promising results of SN6 in the electromyographic behavior of stomatognathic muscles. Always emphasizing that results must be considered very carefully due to the inadequate sample size.
5. Conclusions
It was verified in this pilot study that JFO provides alteration of the resting records in the mandibular rest position of the studied muscles, indicating relaxation of the muscles studied and a more symmetrical electric activity.
Further studies are necessary for a better understanding of the effects of functional orthopedic appliances in the electric activity of stomatognathic muscle in the mandibular rest position.
References
-
J. P. Okeson, Management of Temporomandibular Disorders and Occlusion. Quintessence Publishing, 2019.
-
D. Manfredini, Current Concepts in Temporomandibular Disorders. Quintessence Publishing, 2010.
-
W. R. Proffit, H. W. Fields Jr., and D. M. Sarver, Contemporary Orthodontics. Elsevier, 2018.
-
Mcnamara Jr. and J. A., “Components of class II malocclusion in children 8-10 years of age,” The Angle Orthodontist, Vol. 51, No. 3, pp. 177–202, 1981.
-
T. Yamamoto, M. Kaku, S. Ono, M. Takechi, and K. Tanimoto, “Correction of severe skeletal class ii high angle with mandibular retrusion and gummy smile by double-jaw surgery,” The Bulletin of Tokyo Dental College, Vol. 63, No. 4, pp. 177–187, Jan. 2022, https://doi.org/10.2209/tdcpublication.2022-0016
-
V. Bogdanov, M. Dinkova, and D. Tsakova, “Effect of pre-orthodontic trainer treatment on the masticatory and perioral muscles in patients with class II subdivision 1 malocclusion evaluated by surface EMG,” Folia Medica, Vol. 65, No. 5, pp. 816–820, Oct. 2023, https://doi.org/10.3897/folmed.65.e94741
-
R. C. Carneiro Chagas Tanus and O. Santiago, “Behavior of the mandibular length in class II non-growing patients treated with jaw functional orthopedics,” Jaw Functional Orthopedics and Craniofacial Growth, Vol. 2, No. 3, pp. 151–157, Dec. 2022, https://doi.org/10.21595/jfocg.2022.23008
-
T. Xia, R. Luo, and M. Wang, “Comparison of masticatory myofunctional rehabilitation combined with conventional functional appliances for the treatment of class II, division 1 malocclusion. A retrospective cohort study,” Journal of Stomatology, Oral and Maxillofacial Surgery, Vol. 124, p. 101511, 2023, https://doi.org/10json.1016/j.jormas.2023.101511
-
W. A. Simões, Ortopedia Funzionale Dei Mascellari Attraverso La Riabilitazione Neuro-Occlusale. (in Italian), Trestina, Nike Srl, 2010.
-
E. Sakai, L. W. Ribeiro, O. Santiago Jr., S. P. Terçarolli, and J. G. Amorim, “Determinated Area (DA) treatment goal when treating malocclusions with Jaw Functional Orthopedics (JFO): contribution to scientific evidence,” Journal of Jaw Functional Orhtopedics and Craniofacial Growth, 2024.
-
O. Santiago Júnior, M. V. Lucas Ferreira, and R. Huebner, “Treatment of temporomandibular dysfunction with jaw functional orthopedics: a retrospective study,” Jaw Functional Orthopedics and Craniofacial Growth, Vol. 1, No. 1, pp. 18–27, Jun. 2021, https://doi.org/10.21595/jfocg.2021.22080
-
S. Julious, “Sample size of 12 per group rule of thumb for a pilot study,” Pharmaceutical Statistics: The Journal of Applied Statistics in the Pharmaceutical Industry, Vol. 4, No. 4, pp. 287–291, 2005.
About this article
The authors have not disclosed any funding.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Sergio Polízio Terçarolli – data curation, investigation. Eduardo Sakai – conceptualization, project administration, supervision, writing-review and editing. Michelly Marin P. Sutti – validation and investigation. Stella Travalão Faria Dumke – validation and investigation. Murilo Bovi Corsi – methodology. Orlando Santiago Jr – writing original draft preparation, validation, methodology
The authors declare that they have no conflict of interest.
This research was approved by Universidade Estadual de Campinas (UNICAMP), Piracicaba, Brazil under protocol number 159/2004.

