Abstract
Dentofacial deformities can begin in a very subtle way, which is why there is a need for a well-defined diagnosis. To ascertain whether there is a consensus among specialists regarding the importance of identifying dentofacial deformities in children before they reach six years of age; and to develop and validate a screening tool to assist general dentists so that they can identify signs of craniofacial asymmetry, thereby directing preventive and minimally invasive approaches in children aged three to six years. The guide was created and validated by 37 specialist professionals, masters and doctors. The Delphi technique was used for data analysis, along with the content validity index (CVI) and Cronbach’s alpha. Among the evaluators, 81.08 % had completed their training more than 10 years ago and 78.38% had been working as dentists for more than 10 years; 2.16 % were specialists, 32.16 % had a master's degree and 5.41 % had a doctoral degree. The agreement between the evaluators through the CVI was 100 % and the average Cronbach's alpha was 0.7571, which was considered substantial or acceptable. The clinical semiology guide for detecting dentofacial deformities in children between 3 and 6 years of age was developed and validated.
1. Introduction
Oral health contributes to the quality of physical, psychological and social wellbeing [1]. According to the World Health Organization (WHO), attaining adequate oral health is the gateway to general health, wellbeing and quality of life [2]. The impact of good oral health goes beyond the absence of pain or discomfort, through ensuring self-confidence, socialization, correct chewing and correct pronunciation [3].
Malocclusion, defined as inadequate or abnormal dental alignment constitutes an important oral health problem worldwide [4]. Its prevalence ranges from 11 % to 99 % and may be associated with several factors, including genetic and environmental components [5-8]. It is among the three most prevalent oral health problems, together with dental caries and periodontal diseases [9, 10].
With a view to the possibility of preventing the onset of malocclusion from an early age, healthcare policymakers, as well as pediatricians and dentists, should be asked to develop preventive or early diagnosis and appropriate treatment strategies. Absence of such strategies leads to consequent structural problems that cause tissue lesions and social maladjustment [11, 12].
The relationship between the jaws and, more precisely, existence of balanced occlusion depend on the structural and functional balance of the stomatognathic system. The main functions that influence jaw development, in which the stomatognathic system is involved, are breathing, swallowing and chewing [4]. Jaw and face development depends on the balance between these functions and these are influenced by the morphology of the structures that relate to them and by the central and peripheral nervous system. It is necessary to consider concurrency (timing) and cooperation (synergism) in breathing, sucking and swallowing movements. Disturbance of one of these three perfectly synchronized and interdependent movements invariably affects the other two functions. It needs to be noted that healthy development of children is not possible without perfect basic oral functions [13].
The term facial asymmetry relates to cases that present dimensional differences between the two sides of the face [14]. With increasing numbers of reports of facial asymmetries, prevention of such conditions has become an objective within medicine and jaw functional orthopedics (JFO) [15]. Many newborns have small facial asymmetries that unfortunately do not disappear spontaneously and can worsen. Making an accurate early diagnosis may be the best way to avoid problems in adulthood [16].
A systematic review study aimed at evaluating the available evidence on the effectiveness of early interventions in malocclusion and its impact on craniofacial structure in children under six years of age suggests that early treatments allow better control in the balanced development of the jaws, can improve facial asymmetries and masticatory efficiency [17].
Some authors have recommended that new studies should be conducted in order to evaluate signs of asymmetry rigorously and precisely, so as to be able to make correct diagnoses and subsequently implement early minimally invasive interventions, among patients with facial asymmetry [14, 16-19].
Educational materials and/or materials that assist in clinical practice should be developed, standardized and validated by specialist professionals who are heavily involved in activities within the field in question, always with both a practical and a scientific basis [20].
The objective of this study was to ascertain whether there is a consensus among specialists regarding the importance of identifying and treating dentofacial deformities in children before they reach six years of age; and to develop and validate a guide to assist general dentists so that they can identify signs of dentofacial deformities, thereby directing preventive and minimally invasive approaches in children aged three to six years.
2. Materials and methods
2.1. Elaboration of a guide for identifying signs that may interfere with craniofacial development
A flowchart was drawn up to guide professionals with regard to observing the signs or alterations that may interfere with craniofacial development, Fig. 1.
Step 1: Facial analysis. The professional should take pictures of patients in accordance with standardized guidance for examination of asymmetries. At this stage, the position of the chin, the shape of the orbits, the width of the cheekbones and the bi-commissural plane should be analyzed. In addition, the ears should be evaluated (height, shape and anteroposterior position).
Step 2: Dysfunctions. Possible dysfunctions of the stomatognathic system should be analyzed. At this stage, the type of breathing, lip sealing, presence of non-functional sucking, the tongue and type of feeding should be observed, along with any presence of rhinitis, otitis or adenoid inflammation and whether amygdalectomy or adenoidectomy has been performed.
Step 3: Assessment of teeth. Teeth may show signs of abnormalities relating to chewing and parafunctions. In a balanced mouth, the deciduous teeth are subjected to physiological wear on both sides. If there is more wear on one side than on the other, this can signal the preferential masticatory side (in this case, investigate whether the origin is functional or cranial); excessive wear may be a sign of bruxism. The number of teeth and possible anomalies of the teeth should be analyzed.
Step 4: Static occlusion. Static occlusion can be done just through observation, but photographs enable better analysis. Evaluations of the sagittal relationship and overjet and overbite may point to abnormalities that need to be treated, but do not show whether there is asymmetry. Thus, on the flowchart, there is no alternative that leads to the box of possible cranial alterations.
Midline abnormalities and sagittal differences between the right and left sides are suggestive of cranial alterations. Therefore, if such alterations are presented, the flowchart may lead straight to the box of possible dentofacial deformities.
Step 5: Dynamics of chewing. Analysis on the dynamics of chewing is very important, because this shows whether there is symmetry between movements on the right and left sides and the preferred side for chewing.
Fig. 1Flowchart and guide for the professional to observe signs or alterations that may interfere with craniofacial development
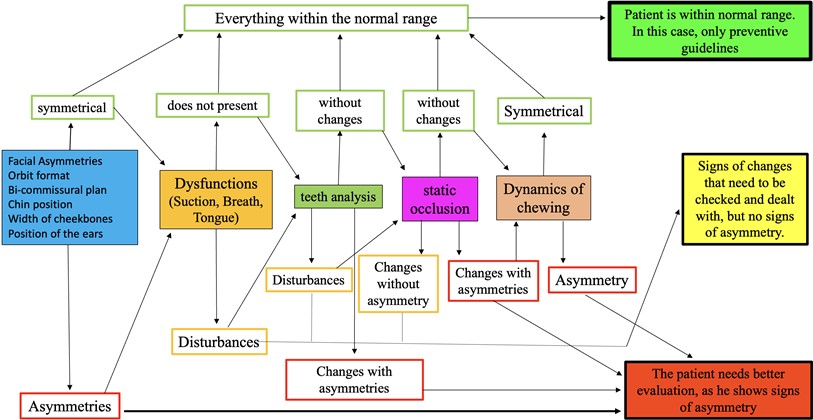
Instructions for carrying out this assessment:
1) To evaluate these dynamics, the child should be asked to chew hard food or even hard gum (food of hard consistency, but little thickness).
2) Give some type of hard food that is not too thick to the child. Ask him or her to chew it a bit on one side. At the moment when the child is biting through it, ask him or her to stop. Displace the child’s lips in order to observe the relationship between the molars. If possible, take a photograph. Repeat this process on the other side.
3) Observe how chewing is done on both the right and left side. Check whether the chewing cycle is the same for both sides. Note whether the child chews by moving the mandible rearwards more on one side than on the other, or whether the child moves it forwards more.
2.2. Summary of the results from the evaluation
According to the responses to the examination questions, three groups will be formed:
1. If all responses point to normality. The patient shows no signs of abnormalities of craniofacial development and has a high chance of attaining balanced development. In this case, the professional must give preventive guidance to the parents or guardians, with the reminder that consultations with a dentist should be sought at least once a year. Preventive guidelines should be drawn up, with regard to hygiene care, chewing that alternates between the right and left sides, use of a diet that includes more fibrous foods, eschewing of possible harmful habits and periodic consultations with a dentist.
2. Signs of alterations that need to be checked and treated, but without signs of asymmetry. For a child to be in this category, there cannot be any signs of asymmetry. On the basis of the examination data, the general dentist should direct this patient to a specialist in this field (pediatric dentistry, orthodontics or functional orthopedics of the jaws).
3. The patient needs better evaluation, because he or she shows signs of asymmetry. Patients who showed signs of asymmetry will be placed in this group. All alterations that point to some functional or structural alteration (with or without signs of asymmetry) that may compromise balanced development of the jaws and/or face will be highlighted in the examination.
2.3. Study location
This study was conducted virtually, and the evaluators answered a questionnaire on Google Drive. The questionnaire consisted of presentation of the protocol followed by multiple-choice questions to assess the subjects’ understanding and validation of the protocol.
2.4. Selection of evaluators
The study was conducted among dentists who were specialists in pediatric dentistry, orthodontics and JFO, with extensive experience in this field. To choose the number of evaluators, the requirements used by Pasquali [21] were followed, which suggested that between six and twenty evaluators should be included. The inclusion criteria for the evaluators were that they should be professionals who reached five points or more.
2.5. Exclusion criteria for evaluators
The following were excluded: professionals who did not reach five points or obtained scores lower than this, according to the items in Chart 1; professionals who agreed to participate in the research, but did not answer the survey questionnaire and/or did not submit answers within the established period of fifteen days; and professionals who withdrew their consent to participate in the research at any time, from the time of their inclusion in the study to the time when the study results became public, even though they had signed a free and informed consent statement.
2.6. Data collection
For validation of the protocol, the following documents were prepared:
1) Invitation/presentation letter, which was sent to the evaluators via email through Google forms.
2) Free and informed consent statement for the evaluators.
3) Evaluator’s declaration of acceptance of participation.
4) Presentation of the protocol and specific criteria.
The invitation letter was composed of an initial personal presentation and elucidations on the research theme, with objective definitions regarding the functional orthopedics of the jaws, the opinion report from the Research Ethics Committee of the “Dr. José Antônio Garcia Coutinho” School of Health Sciences and explanations about the importance of the professionals providing the evaluations in this study. Steps-by-step guidance was given to ensure effective participation by the evaluators, along with notification of the time limit of fifteen days for each round of the evaluation, counting from the day of delivery, for responses to be made and returned.
The free and informed consent statement made it clear to the evaluators what the research consisted of. It guaranteed confidentiality of personal information and emphasized that the evaluators were free to decide whether they wanted or did not want to participate in the research. It also made the participants aware that they had the right to withdraw their consent to participate, at any time. The evaluators were asked to add their name and profession to the statement if they accepted it.
The specific questionnaire was divided into two parts: identification of the evaluator; and evaluation of the protocol. The professionals evaluated the following items of the protocol: thematic content, graphic presentation, vocabulary, sequence, clarity and understanding of the information and description of the clinical examination.
The Likert scale was used in the questions evaluating the protocol, with the following responses: “adequate”, “totally adequate”, “inadequate”, “partially adequate”, “does not apply”. The questions were formulated such that the judges could insert their own opinions and suggestions.
The protocol validation process was as follows:
1. Choice of evaluator professionals: the e-mail or personal contacts of the participants were verified. These evaluators needed to be dentists who were specialists in pediatric dentistry, orthodontics or functional orthopedics of the jaws.
2. The instrument was sent to the evaluators by e-mail, through Google forms, through which the participants could read the free and informed consent statement and could then freely agree to participate.
3. In the data analysis, responses that were marked as category 3 (adequate) or 4 (totally adequate) were considered to be validations. Responses in categories 1 (inadequate) or 2 (partially adequate) and 0 (not applicable) were not excluded. Suggestions presented by the evaluators were considered and reviews were carried out so that the items were then considered validated, and these guidelines were indicated in previous studies on this evaluation method [22-24].
The Delphi technique is a method that has the characteristic of obtaining the opinions of judges with specific knowledge in a given field [24]. It uses questionnaires in which the contents are analyzed and judged by specialists, with the aim of seeking 100 % consensus among the evaluators. This is generally achieved through two to three rounds or evaluation cycles, although there may be more than this [25, 26].
This is a technique in which the results are accounted depending on the degree of specialty, without specifying the number of judges. This technique motivates judges to think more about the matter in question, since they will be its creators [25, 26]. For this process, two groups were used: one executor group, which was composed by the researchers, whose function was to contact the respondents, elaborate the initial questionnaire, analyze the data and elaborate the other questionnaires; and the group formed by the selected judges.
2.7. Ethical issues
The present study followed the norms defined by resolution 466/12 of the National Health Council for research on human beings. It was approved by the Research Ethics Committee of the “Dr. José Antônio Garcia Coutinho” School of Medical Sciences of UNIVÁS (approval opinion report number: 4,390,918)
2.8. Statistical analysis
The data were tabulated in Microsoft Excel 2016 and were then subjected to statistical analysis. Central trend measurements were used for quantitative variables and absolute and relative frequencies for categorical variables. The Minitab software, version 19.1, and the Statistical Package for the Social Sciences software, version 26.0 (SPSS Inc., Chicago, USA), were used. The significance level used as the acceptance or rejection criterion in the statistical tests was 5 % ( 0.05).
Cronbach's alpha coefficient () was applied to analyze the results and assess the internal consistency of the questionnaire. This was first presented by Lee J. Cronbach in 1951 as a way to estimate the reliability of a questionnaire applied in a survey. It analyzes the correlations between respondents’ answers to a questionnaire and presents average correlations between the questions. The α coefficient is calculated from the variance of the individual items and from the variance of the sum of each evaluator’s items, for all the items of a questionnaire that use the same measurement scale [27].
The interpretation of Cronbach's alpha coefficient is apparently intuitive, with values ranging from zero to one. It is then understood that the internal consistency of a questionnaire becomes greater as the value of this statistic comes closer to one. There is much discussion about acceptable alpha values: in general, these range from 0.70 to 0.95.
The practical way to judge the alpha value is to compare the calculated value with the value recommended by different authors in tables presented in the literature. This rule is imprecise, but it serves as a first approximation, provided that the precaution of taking into account the limitations of this statistic is borne in mind. See Tables 1 and 2.
The content validity index (CVI) is used to quantify the degree of agreement between respondents with regard to certain aspects of the instrument and its items. It allows initial analysis on each item individually and then on the instrument as a whole.
Table 1Internal consistency of the questionnaire according to the alpha value (LANDIS and KOCH, 1977)
Alpha value | Internal consistency |
> 0.80 | Almost perfect |
0.80 to 0.61 | Substantial |
0.60 to 0.41 | Moderate |
0.40 to 0.21 | Fair |
< 0.21 | Low |
Table 2Internal consistency of the questionnaire according to the alpha value (GEORGE and MALLERY, 2003; Apud GLIEM; GLIEM 2003)
Alpha value | Internal consistency |
0.91 or more | Excellent |
0.90 to 0.81 | Good |
0.80 to 0.71 | Acceptable |
0.70 to 0.61 | Questionable |
0.60 to 0.51 | Poor |
Less than 0.51 | Unacceptable |
3. Results
Studies show that cases of malocclusion and dentofacial deformities are quite prevalent. However, there was a need for standardization or for an instrument that would help general dentists to diagnose malocclusions and craniofacial asymmetries. After preparation of a protocol, a validation process was undertaken. The participants in this study were specialists in orthodontics, pediatric dentistry and functional orthopedics of the jaws. The questionnaire consisted of two stages: the first of these related to identification of the evaluators (Table 3).
In the second stage, the evaluators answered three questions and their responses were scored from 0 to 4, as follows: 0 (not applicable), 1 (inadequate), 2 (partially adequate), 3 (adequate) and 4 (totally adequate). When asked if the algorithm met the objective of guiding professionals in the clinical examination on patients (Question A), 21.62 % considered this to be adequate and 78.38 % totally adequate (Graph 1A). Regarding the clarity of the algorithm instructions (Question B), 29.73 % and 70.27 % considered that it was adequate and totally adequate, respectively (Graph 1B). Regarding the sequence of information (Question C), 18.92 % considered this to be adequate and 81.08 % totally adequate (Graph 1C). The CVI index, which assesses the degree of agreement among the evaluators, was 100 %.
The overall alpha coefficient of this questionnaire was 0.7571, which was considered to be substantial or acceptable (Table 4). Individual evaluations on the questions showed that Cronbach’s alpha was 0.6067, 0.5879 and 0.7953 for questions A, B and C, respectively (Table 5). Please kindly describe what is the meaning of this results in a way clinicians can understand it
Table 3List of dentists who participated in the validation process for the protocol, in relation to their length of time since completing their training, length of time working and academic titles
Length of time since completing training | ||
Time | Number of professionals | % |
Less than 5 years | 1 | 2.70 |
Between 5 and 10 years | 6 | 16.22 |
More than 10 years | 30 | 81.08 |
Length of time working | ||
Time | Number of professionals | % |
Less than 5 years | 1 | 2.70 |
Between 5 and 10 years | 7 | 18.92 |
More than 10 years | 29 | 78.38 |
Academic titles | ||
Title | Number of professionals | % |
Specialization | 23 | 62.16 |
Master’s | 12 | 32.43 |
Doctorate | 2 | 5.41 |
Fig. 2Percentages of responses among the evaluators when asked: a) Does the protocol meet the objective of guiding professionals in the clinical examination of patients? b) Does it meet the objective of guiding professionals regarding the clarity of the protocol instructions? c) Does it meet the objective of guiding professionals regarding the sequence of information?
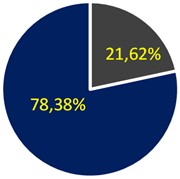
a)
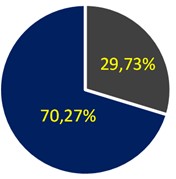
b)
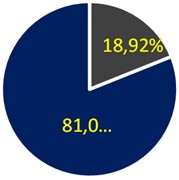
c)
Table 4Result from item and overall statistics with Cronbach’s alpha value
Variable | Total count | Average | Standard deviation |
Question A | 37 | 3.784 | 0.417 |
Question B | 37 | 3.703 | 0.463 |
Question C | 37 | 3.811 | 0.397 |
Total | 37 | 11.297 | 1.051 |
Cronbach’s alpha | 0.7570 | ||
Table 5Result from item statistic omitted, with Cronbach’s alpha value, for questions A, B and C
Variable omitted | Adjusted total average | Adjusted total standard deviation | Adjusted total for item – corrected | Multiple squares – corrected | Cronbach’s alpha |
Question A | 7.5135 | 0.7311 | 0.6471 | 0.4599 | 0.6067 |
Question B | 7.5946 | 0.6855 | 0.6594 | 0.4732 | 0.5879 |
Question C | 7.4865 | 0.8035 | 0.4706 | 0.2218 | 0.7953 |
Higher alpha values suggest that the questionnaire items measure the same construct. The researcher concludes that the questionnaire has internal consistency. In other words, a high Cronbach's alpha coefficient indicates the degree to which the items measure the same construct. The individual values are for the omitted item. For example, if question A is omitted, the alpha value becomes 0.6067. If question B is omitted, the alpha value becomes 0.5879. If question C is omitted, the alpha value becomes 0.7953. It can be concluded that, among the three questions, the most consistent is question B, followed by questions A and C. It is noted that if question C is excluded, the alpha improves.
4. Discussion
If malocclusions and dentofacial deformities are diagnosed before children reach six years of age, the prospects during and after functional orthodontic and/or orthopedic treatment are promising. The diagnostic information obtained is useful for orthodontists, pediatric dentists and functional orthopedists of the jaws and enables them to implement comprehensive care for patients in this age group [17]. However, making an accurate diagnosis is fundamental and professionals often lack specific preparation for doing this [14, 16, 19]. Thus, standardization of guidelines and protocols for correct clinical care, to assist healthcare professionals, becomes necessary [28].
In the present study, clinical semiology guide for detecting dentofacial deformities in children between 3 and 6 years of age was developed and validated in order to direct preventive and minimally invasive approaches. The validation process, sample selection and analysis on the data for this protocol, rigorously delimited guidelines were established with the aim of enabling better conduct and progress of assessments [21-26].
Selection of evaluators for validation of the algorithm is of paramount importance. These judges need to be highly qualified and specialized professionals within the field of activity because they will assess whether the proposed items meet the purposes of the instrument. In theory, 80 % of the evaluators need to come to an agreement, in order to be able to put the need for the study material into objective terms [29]. In the present study, 37 evaluators were selected: most had completed their training more than 10 years previously and had had more than 10 years of clinical practice. It was demonstrated that qualified evaluators were chosen for analyzing the matter in question.
The Delphi technique is used to obtain agreement on a given subject, among specialists within a given field. It has advantages such as anonymity, avoidance of constraints and enablement of feedback from the evaluators, such that they can assist in preparing the material with suggestions. It also enables use of an online process, which allows better reflection, more time for evaluators and lower costs for the researchers [25, 26]. In the present study, the feedback received was positive: nine out of the 37 evaluators presented relevant suggestions for improvement of the algorithm, which were then analyzed. All validation through the Delphi technique was done virtually, thus facilitating the professionals’ access to the algorithm for analysis. This also made it possible to answer the questionnaire at any time, with time for interpretation and reflection.
To assess internal consistency and estimate the reliability of questionnaires applied in research, Cronbach's alpha coefficient () is used. This measures correlations between questionnaire responses, through analysis on the answers given by the respondents, and presents an average correlation between the questions. The coefficient is calculated from the variance of the individual items and the variance of the sum of the items of each evaluator, for all the items of a questionnaire that use the same measurement scale [27, 30]. It is the most widely used analysis method for this purpose [30].
The values of Cronbach’s alpha coefficient can vary between zero and one. The minimum acceptable value is 0.70 because, when values are lower than this, the internal consistency is considered low. The values will at most be 0.90 because higher values may be indicative of redundancy or duplication [30]. In the present study, the value for Cronbach's alpha coefficient was 0.7570, thus indicating acceptable or substantial internal consistency that was within the established limits.
Another factor that influences the alpha value is the length of the questionnaire. If this is very long, the alpha value becomes larger but without this meaning increased internal consistency. A low alpha value may be indicative of only a small number of questions. In situations of redundancy, i.e. when questions are verbalized differently but have practically the same meaning, the alpha value also becomes higher. Lastly, if there are correlations between the questionnaire items, the alpha value will also be higher; and if several items of the questionnaire display correlations with each other, the alpha value will also be higher. Since these correlations are greater when the items of the questionnaire measure the same construct, it can then be concluded that the questionnaire has internal consistency, i.e. high values for Cronbach's alpha coefficient would be indicative for the degree to which the items measure the same construct. Nonetheless, caution is needed because there might be a third variable affecting the responses to any given two items [30].
The CVI was the index indicating agreement among the evaluators of the material in question. It allows each item to be initially analyzed individually, followed by overall analysis of the instrument [29, 31]. When the CVI is 100 %, it means that all evaluators consider that the material under study is relevant for achieving the proposed objective [32-34]. In the present study, the CVI was 100 %, thus validating the protocol and demonstrating that all the evaluators considered that making an early diagnosis of asymmetries is important.
5. Conclusions
The clinical semiology guide for detecting dentofacial deformities in children between 3 and 6 years old was developed and validated with the aim of directing preventive and minimally invasive approaches.
References
-
W. M. Thomson and H. L. Broder, “Oral-health-related quality of life in children and adolescents,” Pediatric Clinics of North America, Vol. 65, No. 5, pp. 1073–1084, Oct. 2018, https://doi.org/10.1016/j.pcl.2018.05.015
-
“Oral health,” World Health Organization, 2021.
-
M. Glick, “The relevance of oral health,” The Journal of the American Dental Association, Vol. 150, No. 8, pp. 637–638, Aug. 2019, https://doi.org/10.1016/j.adaj.2019.06.019
-
M. A. Andrade et al., “Relationship between oclusions and parafunctional habits in early childhood,” Research, Society and Development, Vol. 9, No. 7, p. e484974260, 2020.
-
M. Carotenuto, L. Perillo, M. Esposito, A. Caprioglio, S. Attanasio, and A. C. Santini, “Orthodontic treatment need for adolescents in the Campania region: the malocclusion impact on self-concept,” Patient Preference and Adherence, Vol. 19, No. 8, pp. 353–359, Mar. 2014, https://doi.org/10.2147/ppa.s58971
-
M. Moosazadeh, M. Akbari, K. Lankarani, B. Honarvar, R. Tabrizi, and H. Mirhadi, “Prevalence of malocclusion among Iranian children: A systematic review and meta-analysis,” Dental Research Journal, Vol. 13, No. 5, pp. 387–395, Jan. 2016, https://doi.org/10.4103/1735-3327.192269
-
K. Alvarado, L. López, R. Hanke, R. Picón, and S. Rivas-Tumanyan, “Prevalence of malocclusion and distribution of occlusal characteristics in 13 – to 18-year-old adolescents attending selected high schools in the municipality of San Juan,” Current Health Sciences Journal, Vol. 36, pp. 61–66, 2017.
-
G. Lombardo et al., “Worldwide prevalence of malocclusion in the different stages of dentition: A systematic review and meta-analysis,” European Journal of Paediatric Dentistry, Vol. 21, No. 2, pp. 115–123, Jun. 2020, https://doi.org/10.23804/ejpd.2020.21.02.05
-
E. M. Boeck, K. E. K. C. Pizzol, E. G. P. Barbosa, N. C. A. Pires, and N. Lunardi, “Prevalence of malocclusion in 3 to 6 year-old sucking habit children,” (in Portuguese), Revista de Odontologia da UNESP, Vol. 42, No. 2, pp. 110–116, 2013.
-
M. S. Alhammadi, E. Halboub, M. S. Fayed, A. Labib, and C. El-Saaidi, “Global distribution of malocclusion traits: A systematic review,” Dental Press Journal of Orthodontics, Vol. 23, No. 6, pp. 40.e1–40.e10, Dec. 2018, https://doi.org/10.1590/2177-6709.23.6.40.e1-10.onl
-
R. Lione, M. Buongiorno, G. Laganà, P. Cozza, and L. Franchi, “Early treatment of Class III malocclusion with RME and facial mask: evaluation of dentoalveolar effects on digital dental casts,” European Journal of Paediatric Dentistry: EJPD, Vol. 16, No. 3, pp. 217–220, Sep. 2015.
-
F. D. ’Apuzzo, V. Grassia, V. Quinzi, M. Vitale, G. Marzo, and L. Perillo, “Paediatric Orthodontics Part 4: SEC III protocol in Class III malocclusion,” European Journal of Paediatric Dentistry, Vol. 20, No. 4, pp. 330–334, Jan. 2019, https://doi.org/10.23804/ejpd.2019.20.04.14
-
C. C. G. D. Santos and M. J. P. C. Ferraz, “Atuação da fonoaudiologia na estética facial: relato de caso clínico,” (in Portuguese), Revista CEFAC, Vol. 13, No. 4, pp. 763–768, May 2010, https://doi.org/10.1590/s1516-18462010005000043
-
D. Srivastava, H. Singh, S. Mishra, P. Sharma, P. Kapoor, and L. Chandra, “Facial asymmetry revisited: Part I – diagnosis and treatment planning,” Journal of Oral Biology and Craniofacial Research, Vol. 8, No. 1, pp. 7–14, Jan. 2018, https://doi.org/10.1016/j.jobcr.2017.04.010
-
M. J. Deshayes, “The concept of orthopaedic treatment of facial asymmetry before the age of six,” Cranio-Orofacial Growth Guid. Journal, Vol. 2, No. 1, pp. 2–5, 2014.
-
M.-J. Deshayes, “Dentofacial Orthopedics to treat facial asymmetries before six years of age. How to balance craniofacial growth and enhance temporomandibular function,” L’Orthodontie Française, Vol. 81, No. 3, pp. 189–207, Aug. 2010, https://doi.org/10.1051/orthodfr/2010021
-
P. Valério, T. Poklepović Peričić, A. Rossi, C. Grippau, J. D. S. Tavares Campos, and I. J. Borges Do Nascimento, “The effectiveness of early intervention on malocclusion and its impact on craniofacial growth: A systematic review,” Contemporary Pediatric Dentistry, Vol. 2, No. 2, pp. 1–18, Aug. 2021, https://doi.org/10.51463/cpd.2021.61
-
V. D. ’Ambrosio et al., “Fetal tongue posture associated with micrognathia: An ultrasound marker of cleft secondary palate?,” Journal of Clinical Ultrasound, Vol. 48, No. 1, pp. 48–51, Oct. 2019, https://doi.org/10.1002/jcu.22784
-
A. Paino-Sant’Ana, B. D. R. Fernandes, D. L. Marchiori, and G. M. D. Santos, “Assimetria facial: um desafio para o Cirurgião Ortognata,” (in Portuguese), Archives of Health Investigation, Vol. 10, No. 5, pp. 848–850, May 2021, https://doi.org/10.21270/archi.v10i5.5431
-
G. M. Salomé and C. A. Da Rocha, “Aplicativo móvel para avaliação, prevenção e tratamento da dermatite associada à incontinência,” (in Poruguese), Revista Enfermagem Contemporânea, Vol. 10, No. 1, pp. 8–16, Dec. 2020, https://doi.org/10.17267/2317-3378rec.v10i1.2963
-
L. Pasquali, Instrumentos psicológicos: manual prático de elaboração. (in Portuguese), Brasília: LabPAM/IBAPP, 1999.
-
A. Filgueiras et al., “Translation and semantic adaptation of the attentional control scale for the Brazilian context,” (in Portuguese), Estudos de Psicologia (Campinas), Vol. 32, No. 2, pp. 173–185, Jun. 2015, https://doi.org/10.1590/0103-166x2015000200003
-
M. B. Silveira, R. P. Saldanha, J. C. C. Leite, T. O. F. D. Silva, T. Silva, and L. I. Filippin, “Construction and validation of content of one instrument to assess falls in the elderly,” (in Portuguese), Einstein (São Paulo), Vol. 16, No. 2, Jun. 2018, https://doi.org/10.1590/s1679-45082018ao4154
-
R. L. Palmeira, D. de Lima, and M. S. P. Franco Adriano, “Criação e validação de um instrumento de acompanhamento de egressos do ensino profissional e tecnológico,” (in Portuguese), Práxis Educacional, Vol. 16, No. 41, pp. 367–388, Sep. 2020, https://doi.org/10.22481/praxisedu.v16i41.6423
-
L. D. N. Rodrigues, A. D. S. Santos, P. P. S. Gomes, W. C. P. D. Silva, and E. M. C. Chaves, “Construction and validation of an educational booklet on care for children with gastrostomy,” (in Portuguese), Revista Brasileira de Enfermagem, Vol. 73, No. 3, Jan. 2020, https://doi.org/10.1590/0034-7167-2019-0108
-
M. R. D. Silva and R. C. I. Montilha, “Contribuições da técnica Delphi para a validação de uma avaliação de terapia ocupacional em deficiência visual,” (in Portuguese), Cadernos Brasileiros de Terapia Ocupacional, Vol. 29, Jan. 2021, https://doi.org/10.1590/2526-8910.ctoao2163
-
J. Martin Bland and D. Altman, “Statistical methods for assessing agreement between two methods of clinical measurement,” The Lancet, Vol. 327, No. 8476, pp. 307–310, Feb. 1986, https://doi.org/10.1016/s0140-6736(86)90837-8
-
G. M. Salome and M. A. Pereira Da Silva, “Construção e validação de um manual de prevenção do pé diabético,” (in Portuguese), Saúde (Santa Maria), Vol. 47, No. 1, Mar. 2021, https://doi.org/10.5902/2236583442320
-
R. Medeiros, M. Júnior, D. Pinto, A. Vitor, V. Santos, and E. Barichello, “Pasquali’s model of content validation in the Nursing researches,” (in Portuguese), Revista de Enfermagem Referência, Vol. 4, No. 4, pp. 127–135, Mar. 2015, https://doi.org/10.12707/riv14009
-
R. M. Miranda and M. A. R. Santos, “Avaliação da confiabilidade dos questionários sobre a análise de desempenho de uma escola pública: uma aplicação do alfa de cronbach,” (in Pourtuguese), Revista Produção Industrial and Serviços, Vol. 3, No. 2, pp. 50–61, 2017.
-
R. P. P. Honório, J. Caetano, and P. C. Almeida, “Validation of standard operating procedures in nursing care of patients with totally implanted catheters,” (in Portuguese), Revista Brasileira de Enfermagem, Vol. 64, No. 5, pp. 882–889, Oct. 2011, https://doi.org/10.1590/s0034-71672011000500013
-
F. T. P. Hortense, C. D. Bergerot, and E. B. L. Domenico, “Construction and validation of clinical contents for development of learning objects,” Revista Brasileira de Enfermagem, Vol. 71, No. 2, pp. 306–313, Apr. 2018, https://doi.org/10.1590/0034-7167-2016-0622
-
L. M. M. Sabino et al., “Elaboration and validation of a reader on childhood diarrhea prevention,” Acta Paulista de Enfermagem, Vol. 31, No. 3, pp. 233–239, Jun. 2018, https://doi.org/10.1590/1982-0194201800034
-
G. M. Salomé and N. F. Alves, “App “SICKSEG” in mobile platforms for the prevention of skin injuries,” Revista de Enfermagem UFPE on line, Vol. 14, Apr. 2020, https://doi.org/10.5205/1981-8963.2020.244152
About this article
The authors have not disclosed any funding.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
The initial manuscript and drawings were made by Valéria Medau and Marie Josèphe Deshayes, the scientific methodology was guided by professors Paulo Roberto Maia and José Dias da Silva Neto. Almiro José Machado Júnior helped with the manuscript for this article and the advisor for the entire work was José Dias da Silva Neto. All authors read and approved the final manuscript.
The authors declare that they have no conflict of interest.
The present study followed the norms defined by resolution 466/12 of the National Health Council for research on human beings. It was approved by the Research Ethics Committee of the “Dr. José Antônio Garcia Coutinho” School of Medical Sciences of UNIVÁS (approval opinion report number: 4,390,918).
