Abstract
Temporomandibular disorder (TMD) comprises a group of dysfunctions of the masticatory system involving joint, myofascial, and even sensory alterations. The main symptom of TMD is orofacial pain, which has a negative impact on the quality of life of TMD sufferers, affecting their productivity at work and school, the quality of their sleep, their appetite, and their satisfaction with life. An alternative for the treatment of TMD is the low-level laser therapy (LLLT), which stimulates cellular functions and promotes therapeutic effects. However, there is no consensus in the literature. Objective: This review aimed to elucidate the parameters of low-level laser therapy in the treatment of orofacial pain in patients with temporomandibular disorder. Methods: A search was carried out for scientific articles published between 2013 and 2023 in the MEDLINE, PEDro, LILACS and SciELO databases. Results: A total of 21 studies were previously selected and after the eligibility criteria, 10 studies were included. Can be suggest a protocol for treating patients with temporomandibular disorder by low-level laser therapy with the following parameters: infrared wavelength, energy density less than 10 J/cm2, output power from 100 to 250 mW and at least 8 sessions of treatment. Conclusion: The low-level laser therapy improves orofacial pain in patients with temporomandibular disorder.
1. Introduction
Temporomandibular disorder (TMD) is a generic term that involves a group of disorders of the masticatory system and can be divided into intra-articular or muscular alterations [1]. A common cause of orofacial and neck pain, TMD is considered a public health problem that affects 5 % to 12 % of the world’s population [2].
TMD is the second most common cause of musculoskeletal pain. The main consequence is the impact on the patient’s quality of life, with pain-related disability being one of the chronic conditions observed in the population [3]. The prevalence of TMD is in the 20-40 age group, and it is twice as common in women as in men [4].
The etiology of TMD is multifactorial and is related to functional, structural, and psychological factors, as well as biological, environmental, social, emotional and cognitive triggers [5]. Factors consistently associated with TMD include tension headache, emotional stress and signs of anxiety and depression [6].
The main symptom of TMD is orofacial pain, which is an unpleasant subjective impression that is difficult to describe and measure. It usually corresponds to a manifestation that emerges from an initial spontaneous or provoked injury, communicating it to the central and peripheral nervous system [7]. Other symptoms include clicking, crackling, headache and ringing in the ears [8].
The therapeutic approach to TMD consists of conservative procedures such as pharmacotherapy, occlusal splints, kinesiotherapy, electrotherapy and laser therapy [9]. Among the various modalities, low-level laser therapy (LLLT) has recently been highlighted for being non-invasive, athermic, easy to apply, cost-effective, with shorter treatment times and no side effects [10].
Low-level laser is a phototherapy resource that emits electromagnetic radiation in the red to near-infrared spectral range (600-1000 nm), with low energy densities that stimulate cellular functions and promote therapeutic effects [11]. In terms of physiological effects, this light promotes increased ATP production, increased fibroblast proliferation and collagen synthesis, increased RNA and DNA synthesis, stimulated angiogenesis and induced changes in nociceptive afferents [12].
Orofacial pain has a negative impact on the quality of life of TMD sufferers, impairing their productivity at work, in college, the quality of their sleep, their appetite and satisfaction with life. Although there are many studies reporting the effects of low-level laser on TMD [13, 14], there is still no consensus in the literature on the ideal parameters for treating orofacial pain. Therefore, this study aimed to elucidate the parameters of the low-level laser therapy in the treatment of orofacial pain in patients with temporomandibular disorder.
2. Methods
This is a narrative review. A search was carried out in the Medline, PEDro, LILACS and SciELO databases. The search was limited to articles published in English and Portuguese between 2013 and 2023. The keywords “disfunção temporomandibular”, “dor orofacial”, “laser de baixa intensidade”, “tratamento”, “temporomandibular disorder”, “orofacial pain”, “low-level laser therapy” and “treatment” were used.
The inclusion criteria defined were randomized clinical trials that addressed low-level laser in the treatment of orofacial pain in individuals of both sexes and with a diagnosis of TMD classified based on the DC/TMD protocol (Diagnostic Criteria for Temporomandibular Disorder). This protocol was published by TMD specialists for epidemiological and clinical data with the dual axis system: axis I which included a physical assessment using reliable and well operationalized diagnostic criteria, and axis II which refers to psychosocial status and pain-related disability. This protocol has been updated and has become an evidence-based assessment and diagnostic tool [15].
The exclusion criteria were studies that used analgesics, anti-inflammatories or included therapeutic techniques such as transcutaneous electrical nerve stimulation (TENS), ultrasound, acupuncture, ozone therapy, myofascial release, manual therapy associated with laser in the treatment of TMD.
3. Results and discussion
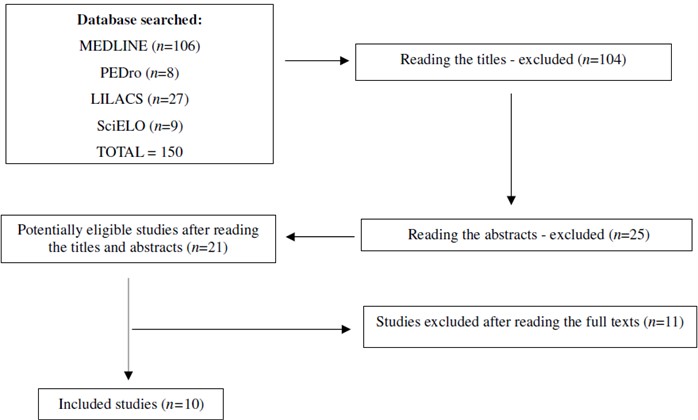
After searching the scientific databases, 150 studies were identified, excluding publications unrelated to the topic. Of the 21 selected, 10 studies were included in this review (Fig. 1).
The studies included show an adult population with a diagnosis of temporomandibular disorder in their sample, based on the DC/TMD (Diagnostic Criteria for Temporomandibular Disorder) protocol. These studies are described in Table 1.
The age of individuals with TMD ranged from 18 to 76 years, with a predominance in the 25 to 45 age group. These data corroborate Valesan et al. [2] who confirmed that the peak incidence of TMD is between 20 and 40 years of age. Up to the age of 40, the most frequent causes of TMD are of muscular origin and, from this age onwards, of articular origin.
The studies showed a predominance of females. According to the literature, women are twice as affected by TMD as men [26]. This predisposition is linked to factors that contribute to the differences between the sexes, such as hormonal, cultural, social, emotional stress, pain threshold and sensitivity [27, 28]. Therefore, the population’s sample profile of the included studies was young women.
According to Ren et al. [29] the most prevalent symptom in TMD sufferers is orofacial pain. Of the 10 studies, 9 used the Visual Analog Scale (VAS) to measure pain intensity before and after laser intervention. This scale ranges from 0 (no pain) to 10 (maximum pain), thus fulfilling a requirement of the American Dental Association, which recommends that pain in the TMJ and masticatory muscles be measured by palpating these structures and recorded on a pain scale. Hanna et al. [28] state that simple assessment scales such as the Visual Numeric Scale (VNS) or VAS have been considered the most reliable tools for assessing pain intensity in clinical practice.
Fig. 1Flowchart of study selection
With regard to the application parameters of the low-level laser, 9 studies applied the wavelength in the near-infrared range within the electromagnetic radiation spectrum, i.e. above 750 nm [11]. This finding is consistent with the literature, which points to the wavelength of laser light in the infrared range as being effective in reducing TMD-related orofacial pain [30].
The energy density used in the studies ranged from 2.8 J/cm2 to 21 J/cm2, with a predominance of values below 10 J/cm2. The output power varied from 20 mW to 300 mW, with a predominance in the 100 to 250 mW. These results are in line with the review by Tuner et al [31], in which the authors state that low-level laser at a wavelength of 800 nm to 900 nm, output power of 100 mW to 500 mW and energy density of less than 10 J/cm2 promoted analgesia and improved mandibular movements in patients with TMD. Furthermore, according to the Arndt-Schulz law, lower doses produce photobiostimulation and higher doses produce photobioinhibition [32].
The application time per laser spot varied from 8 seconds to 120 seconds. The treatment varied from 1 to 12 sessions, with the most studies having at least 8 sessions. According to Santos et al. [33], some factors directly affect the results of laser application, such as wavelength, power output of the device, application time and frequency of sessions. Despite the divergence of these low-level laser application parameters, the therapeutic effects were not compromised in TMD.
Using the parameters applied, all the studies showed a significant reduction in orofacial pain in TMD patients after treatment with low-level laser therapy. These results corroborate the findings of Ferrillo et al. [34], who point to the biological effects of low-level laser as reducing inflammatory cytokines and raising the pain threshold by affecting cell membrane potential. These effects provide analgesia in TMD patients.
Some studies have also shown a reduction in orofacial pain in the placebo group. Similarly, in the review by Argueta-Figueroa et al. [35], some studies showed no difference between the laser and placebo groups in pain reduction. Because it is an individual experience, pain itself is a critical factor in the development of neurochemical analgesic response, which justifies placebo analgesia.
Based on included studies, can be suggest a protocol for treating patients with temporomandibular disorder by low-level laser therapy. The following laser parameters are recommended: wavelength above 750 nm, energy density less than 10 J/cm2, output power from 100 mW to 250 mW and at least 8 sessions.
Table 1Characteristics of included studies
Study | Sample | Intervention | Assessment tool | Main results |
Ferreira et al. [16] | n = 40 G1 = 20 G2 = 20 Age (average): G1 = 32.2 years G2 = 36.2 years Sex: 40 F | G1- Laser 780 nm, 4.5 J/cm2, 50 mW, 90 s per point. G2- Placebo laser. 12 sessions | VAS | G1 achieved total pain remission after treatment (0.05). G2 had a decrease in pain intensity after treatment (0.05). |
Ahrari et al. [17] | n = 20 G1 = 10 G2 = 10 Age (average): 35.5 years Sex: 20 F | G1- Laser 810 nm, 3.4 J/cm2, 50 mW, 120 s per point. G2- Placebo laser. 12 sessions | VAS | G1 obtained a significant reduction in pain intensity (0.05). G2 had an alternation between improvement and worsening of pain, with no significant reduction (0.05). |
Sancakli et al. [18] | n = 30 G1 = 10 G2 = 10 G3 = 10 Age (average): 39.2 years Sex: 9 M / 21 F | G1- 820 nm laser, 3 J/cm2, 300 mW, 10 s per point. G2- 820 nm laser, 3 J/cm2, 300 mW, 10 s per point. G3- Placebo laser. 12 sessions | VAS | G1 and G2 had a significant reduction in pain intensity (0.05) pre- and post-treatment. G3 had no significant reduction in pain intensity (0.05) pre- and post-treatment. |
Costa et al. [19] | n = 60 G1 = 30 G2 = 30 Age (average): 38.8 years Sex: 6 M / 54 F | G1- 830 nm laser, 2.8 J/cm2, 100 mW, 28 s per point. G2- Placebo laser. 1 session | VAS | G1 and G2 had no significant reduction in pain intensity (0.05) pre- and post-treatment, using the VAS. G1 had a significant reduction in pain intensity (0.05) through palpation of the points. |
Shobha et al. [20] | n = 40 G1 = 20 G2 = 20 Age (average): G1 = 30.8 years G2 = 27.5 years Sex: 9 M / 31 F | G1- Laser 810 nm, 6 J/cm2, 100 mW 60 s per point. G2- Placebo laser. 8 sessions | VAS | G1 and G2 had a significant reduction in pain intensity (0.05). |
Madani et al. [21] | n = 45 G1 = 15 G2 = 15 G3 = 15 Age (average): 38 years Sex: 12 M / 33 F | G1- Laser 810 nm, 21 J/cm2, 200 mW, 30 s per point. G2- Laser acupuncture points, 810 nm, 21 J/cm2, 200 mW, 30 s per point. G3- Placebo laser. 10 sessions | VAS | G1 and G2 had a significant reduction in pain intensity (0.05), and G3 did not. |
Monteiro et al. [22] | n = 42 G1 = 22 G2 = 20 Age (average): G1 = 29.1 years G2 = 25.6 years Sex: 10 M / 32 F | G1- Laser 635 nm, 8 J/cm2, 200 mW, 20 s per point. G2- Placebo laser. 4 sessions | VAS | G1 had a significant reduction in pain intensity (0.05) pre- and post-treatment. G2 had no significant reduction in pain intensity (0.05) pre- and post-treatment. |
Aisaiti et al. [23] | n = 100 G1 = 25 G2 = 25 G3 = 25 G4 = 25 Age (average): G1 = 34.8 years G2 = 33.2 years G3 = 35 years G4 = 34.8 years Sex: 24 M / 76 F | Arthralgia groups: G1- Laser 810 nm, 6 J/cm2, 100 mW, 30 s per point. G2- Placebo laser. Myalgia groups: G3- 810 nm laser, 6 J/cm2, 100 mW, 20 s per point. G4- Placebo laser. 7 sessions | VAS | All groups had a significant reduction in pain intensity (0.05), with a greater reduction in G1 and G3. |
Del Vecchio et al. [24] | n = 86 G1 = 29 G2 = 28 G3 = 29 Age (average): 42.5 years Sex: 12 M / 74 F | G1- Laser 808 nm, 8 J/cm2, 250 mW, 8 s per point. G2- Placebo laser. G3 - Medication. 7 sessions | VAS | G1 and G3 had a significant reduction in pain intensity (0.05), and G2 did not. |
Magri et al. [25] | n = 41 G1 = 20 G2 = 21 Age (average): G1 = 32.7 years G2 = 29.8 years Sex: 41 F | G1- Laser 780 nm, 5 J/cm2, 20 mW, 10 s per point. G2- Placebo laser. 8 sessions | VAS | G1 and G2 had a significant reduction in pain intensity (0.05). |
M = male, F = female, S = seconds, VAS = visual analog scale | ||||
4. Conclusions
This review suggests the best low-level laser parameters to reduce orofacial pain are infrared wavelength, dosage of < 10 J/cm2, output power from 100 to 250 mW and at least 8 sessions of treatment. New randomized clinical trials should be carried out in an attempt to standardize the application parameters of the low-level laser therapy and thus promote greater reliability for the technique in temporomandibular disorder.
References
-
J. Lomas, T. Gurgenci, C. Jackson, and D. Campbell, “Temporomandibular dysfunction,” Australian Journal of General Practice, Vol. 47, No. 4, pp. 212–215, Apr. 2018, https://doi.org/10.31128/afp-10-17-4375
-
L. F. Valesan et al., “Prevalence of temporomandibular joint disorders: a systematic review and meta-analysis,” Clinical Oral Investigations, Vol. 25, No. 2, pp. 441–453, Jan. 2021, https://doi.org/10.1007/s00784-020-03710-w
-
F. R. Carvalho, R. Q. Barros, A. S. Gonçalves, and P. M. Freitas, “Photobiomodulation therapy on the palliative care of temporomandibular disorder and orofacial/cervical skull pain: study protocol for a randomized controlled clinical trial,” Trials, Vol. 20, No. 1, pp. 200–208, Apr. 2019, https://doi.org/10.1186/s13063-019-3294-7
-
R. Akhter, “Epidemiology of temporomandibular disorder in the general population: a systematic review,” Advances in Dentistry and Oral Health, Vol. 10, No. 3, pp. 1–13, Feb. 2019, https://doi.org/10.19080/adoh.2019.10.555787
-
D. T. S. Li and Y. Y. Leung, “Temporomandibular disorders: current concepts and controversies in diagnosis and management,” Diagnostics, Vol. 11, No. 3, p. 459, Mar. 2021, https://doi.org/10.3390/diagnostics11030459
-
V. P. Natu, A. U. J. Yap, M. H. Su, N. M. Irfan Ali, and A. Ansari, “Temporomandibular disorder symptoms and their association with quality of life, emotional states and sleep quality in South‐East Asian youths,” Journal of Oral Rehabilitation, Vol. 45, No. 10, pp. 756–763, Aug. 2018, https://doi.org/10.1111/joor.12692
-
M. Ferrillo et al., “Pain management and rehabilitation for central sensitization in temporomandibular disorders: a comprehensive review,” International Journal of Molecular Sciences, Vol. 23, No. 20, p. 12164, Oct. 2022, https://doi.org/10.3390/ijms232012164
-
J. Fehrenbac, B. S. G. Silva, and L. P. Brondani, “The association of temporomandibular dysfunction with orofacial pain and headache,” Journal of Oral Investigations, Vol. 7, No. 2, pp. 69–78, 2018.
-
J. Chen, Z. Huang, M. Ge, and M. Gao, “Efficacy of low‐level laser therapy in the treatment of TMDs: a meta‐analysis of 14 randomised controlled trials,” Journal of Oral Rehabilitation, Vol. 42, No. 4, pp. 291–299, Dec. 2014, https://doi.org/10.1111/joor.12258
-
G.-Z. Xu, J. Jia, L. Jin, J.-H. Li, Z.-Y. Wang, and D.-Y. Cao, “Low-level laser therapy for temporomandibular disorders: a systematic review with meta-analysis,” Pain Research and Management, Vol. 2018, pp. 1–13, Jan. 2018, https://doi.org/10.1155/2018/4230583
-
H. Chung, T. Dai, S. K. Sharma, Y.-Y. Huang, J. D. Carroll, and M. R. Hamblin, “The nuts and bolts of low-level laser (light) therapy,” Annals of Biomedical Engineering, Vol. 40, No. 2, pp. 516–533, Nov. 2011, https://doi.org/10.1007/s10439-011-0454-7
-
V. Mansouri, B. Arjmand, M. Rezaei Tavirani, M. Razzaghi, M. Rostami-Nejad, and M. Hamdieh, “Evaluation of efficacy of low-level laser therapy,” Journal of Lasers in Medical Sciences, Vol. 11, No. 4, pp. 369–380, Oct. 2020, https://doi.org/10.34172/jlms.2020.60
-
S. A. Ahmad, S. Hasan, S. Saeed, A. Khan, and M. Khan, “Low-level laser therapy in temporomandibular joint disorders: a systematic review,” Journal of Medicine and Life, Vol. 14, No. 2, pp. 148–164, Mar. 2021, https://doi.org/10.25122/jml-2020-0169
-
A. Sobral et al., “Photobiomodulation and myofascial temporomandibular disorder: systematic review and meta-analysis followed by cost-effectiveness analysis,” Journal of Clinical and Experimental Dentistry, Vol. 13, No. 7, pp. e724–e732, Jan. 2021, https://doi.org/10.4317/jced.58084
-
E. Schiffman et al., “Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: recommendations of the international RDC/TMD consortium network and orofacial pain special interest group,” Journal of Oral and Facial Pain and Headache, Vol. 28, No. 1, pp. 6–27, Jan. 2014, https://doi.org/10.11607/jop.1151
-
L. A. Ferreira, R. G. de Oliveira, J. P. Guimarães, A. C. P. Carvalho, and M. V. Q. de Paula, “Laser acupuncture in patients with temporomandibular dysfunction: a randomized controlled trial,” Lasers in Medical Science, Vol. 28, No. 6, pp. 1549–1558, Feb. 2013, https://doi.org/10.1007/s10103-013-1273-x
-
F. Ahrari, A. S. Madani, Z. S. Ghafouri, and J. Tunér, “The efficacy of low-level laser therapy for the treatment of myogenous temporomandibular joint disorder,” Lasers in Medical Science, Vol. 29, No. 2, pp. 551–557, Jan. 2013, https://doi.org/10.1007/s10103-012-1253-6
-
E. Sancakli, B. Gökçen-Röhlıg, A. Balık, D. Öngül, S. Kıpırdı, and H. Keskın, “Early results of low-level laser application for masticatory muscle pain: a double-blind randomized clinical study,” BMC Oral Health, Vol. 15, No. 1, pp. 1–6, Oct. 2015, https://doi.org/10.1186/s12903-015-0116-5
-
S. A. P. Costa et al., “The analgesic effect of photobiomodulation therapy (830 nm) on the masticatory muscles: a randomized, double-blind study,” Brazilian Oral Research, Vol. 31, pp. 1–10, Dec. 2017, https://doi.org/10.1590/1807-3107bor-2017.vol31.0107
-
R. Shobha, V. Narayanan, B. Jagadish Pai, H. Jaishankar, and M. Jijin, “Low-level laser therapy: A novel therapeutic approach to temporomandibular disorder – A randomized, double-blinded, placebo-controlled trial,” Indian Journal of Dental Research, Vol. 28, No. 4, p. 380, Jan. 2017, https://doi.org/10.4103/ijdr.ijdr_345_15
-
A. Madani, F. Ahrari, A. Fallahrastegar, and N. Daghestani, “A randomized clinical trial comparing the efficacy of low-level laser therapy (LLLT) and laser acupuncture therapy (LAT) in patients with temporomandibular disorders,” Lasers in Medical Science, Vol. 35, No. 1, pp. 181–192, Aug. 2019, https://doi.org/10.1007/s10103-019-02837-x
-
L. Monteiro, R. Ferreira, T. Resende, J. J. Pacheco, and F. Salazar, “Effectiveness of photobiomodulation in temporomandibular disorder-related pain using a 635 nm diode laser: a randomized, blinded, and placebo-controlled clinical trial,” Photobiomodulation, Photomedicine, and Laser Surgery, Vol. 38, No. 5, pp. 280–288, May 2020, https://doi.org/10.1089/photob.2019.4730
-
A. Aisaiti et al., “Effect of photobiomodulation therapy on painful temporomandibular disorders,” Springer Science and Business Media LLC, Scientific Reports, Apr. 2021.
-
A. Del Vecchio et al., “Evaluation of the efficacy of a new low-level laser therapy home protocol in the treatment of temporomandibular joint disorder-related pain: a randomized, double-blind, placebo-controlled clinical trial,” The Journal of Craniomandibular and Sleep Practice, Vol. 39, No. 2, pp. 141–150, Mar. 2021, https://doi.org/10.1080/08869634.2019.1599174
-
L. V. Magri, C. Bataglion, and C. R. A. Leite-Panissi, “Follow-up results of a randomized clinical trial for low-level laser therapy in painful TMD of muscular origins,” The Journal of Craniomandibular and Sleep Practice, Vol. 39, No. 6, pp. 502–509, Nov. 2021, https://doi.org/10.1080/08869634.2019.1673588
-
C. H. Bueno, D. D. Pereira, M. P. Pattussi, P. K. Grossi, and M. L. Grossi, “Gender differences in temporomandibular disorders in adult populational studies: A systematic review and meta‐analysis,” Journal of Oral Rehabilitation, Vol. 45, No. 9, pp. 720–729, Jun. 2018, https://doi.org/10.1111/joor.12661
-
C. M. Visscher et al., “Comorbid disorders and sociodemographic variables in temporomandibular pain in the general Dutch population,” Journal of Oral and Facial Pain and Headache, Vol. 29, No. 1, pp. 51–59, Jan. 2015, https://doi.org/10.11607/ofph.1324
-
R. Hanna, S. Dalvi, R. J. Bensadoun, and S. Benedicenti, “Role of photobiomodulation therapy in modulating oxidative stress in temporomandibular disorders. a systematic review and meta-analysis of human randomised controlled trials,” Antioxidants, Vol. 10, No. 7, p. 1028, Jun. 2021, https://doi.org/10.3390/antiox10071028
-
H. Ren, J. Liu, Y. Liu, C. Yu, G. Bao, and H. Kang, “Comparative effectiveness of low‐level laser therapy with different wavelengths and transcutaneous electric nerve stimulation in the treatment of pain caused by temporomandibular disorders: A systematic review and network meta‐analysis,” Journal of Oral Rehabilitation, Vol. 49, No. 2, pp. 138–149, Aug. 2021, https://doi.org/10.1111/joor.13230
-
L. R. Furquim et al., “Application of photobiomodulation for chronic pain-related TMD on pain points versus pre-established points: randomized clinical trial,” Journal of Photochemistry and Photobiology B: Biology, Vol. 238, p. 112612, Jan. 2023, https://doi.org/10.1016/j.jphotobiol.2022.112612
-
J. Tunér, S. Hosseinpour, and R. Fekrazad, “Photobiomodulation in temporomandibular disorders,” Photobiomodulation, Photomedicine, and Laser Surgery, Vol. 37, No. 12, pp. 826–836, Dec. 2019, https://doi.org/10.1089/photob.2019.4705
-
Y.-Y. Huang, A. C.-H. Chen, J. D. Carroll, and M. R. Hamblin, “Biphasic dose response in low level light therapy,” Dose-Response, Vol. 7, No. 4, pp. dose–response.0, Oct. 2009, https://doi.org/10.2203/dose-response.09-027.hamblin
-
N. E. B. D. Santos et al., “Low-power laser use for treatment of temporomandibular muscle dysfunction: a systematic review,” Brazilian Journal of Health Review, Vol. 3, No. 6, pp. 18331–18341, Jan. 2020, https://doi.org/10.34119/bjhrv3n6-231
-
M. Ferrillo et al., “Efficacy of rehabilitation on reducing pain in muscle-related temporomandibular disorders: a systematic review and meta-analysis of randomized controlled trials,” Journal of Back and Musculoskeletal Rehabilitation, Vol. 35, No. 5, pp. 921–936, Sep. 2022, https://doi.org/10.3233/bmr-210236
-
L. Argueta-Figueroa, L. A. Flores-Mejía, B. X. Ávila-Curiel, B. I. Flores-Ferreyra, and R. Torres-Rosas, “Nonpharmacological interventions for pain in patients with temporomandibular joint disorders: a systematic review,” European Journal of Dentistry, Vol. 16, No. 3, pp. 500–513, Mar. 2022, https://doi.org/10.1055/s-0041-1740220
About this article
The authors have not disclosed any funding.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Maria Emília De Abreu Chaves: conceptualization, data curation, investigation, methodology, project administration, supervision, validation, visualization, writing-review and editing. Mônica Goulart Fonseca: conceptualization, data curation, investigation, methodology, validation, visualization, writing-original draft preparation. Aline Beatriz Ferreira: conceptualization, data curation, investigation, methodology, validation, visualization, writing-original draft preparation.
The authors declare that they have no conflict of interest.
This study is a review.
