Abstract
X-rays and tomography, in their different modalities, are used as auxiliary diagnostic elements in temporomandibular joint (TMJ) dysfunction, both in static and dynamic situations; however, because they only allow the observation of bone structures, magnetic resonance imaging (MRI) is the ideal method to analyze, among other structures, the articular disc. Among the internal disorders of the TMJ are the abnormal postural relationships between the disc, mandibular head, fossa and articular tubercle, which can even lead to a musculoskeletal condition causing noise, pain and functional limitation. The clinical evaluation of temporomandibular dysfunctions is complex, especially in asymptomatic patients; the Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD), place these entities within the AXIS I protocol, considering that the image is not strictly necessary. However, analyzing the disc situation statically and dynamically, with its surroundings, allows considering the loads that generate dysfunction, leading to the correct diagnosis, and selection of the best treatment. A clinical case is presented, an asymptomatic patient, without functional limitation, who reported a history of occasional mouth opening locking upon awakening. MRI was indicated, finding an abnormal position of the disc, in a static and dynamic situation; finding anterior displacement of the disc in the right and left TMJ in closed mouth position, dynamically anterior displacement without recapture in the right TMJ and with recapture in the left TMJ; Treatment was performed with Jaw Functional Orthopedics (JFO), obtaining changes in the dynamic disc-mandibular head relationship, anterior displacement with recapture of the right TMJ and total recapture of the left TMJ.
1. Introduction
Biomechanically TMJ is a diarthrosis that allows two types of movements: rotation or hinge (ginglymoid) and sliding or translation (arthrodial). The rotation movement is performed by the mandibular head -disc complex, and the translation movement is given by the sliding of this structure over the articular fossa-eminence [1], [2].
The mandibular dynamics take place on different spatial planes and around multiple rotational axes, with temporomandibular joints (TMJs) being responsible for them; and where the articular disc plays an important role in compensating for the inconsistencies of the bone surfaces involved. [1] This is due to its histological composition of fibrous cartilaginous tissue, which in turn is formed by cells and extracellular matrix. These cells, chondrocytes, and fibroblasts, are distributed differently depending on the area of the disc. The most abundant collagen fibers in the articular disc are type I, which are the ones that give the tissues the qualities of elasticity and resistance; while elastin fibers are arranged parallel to collagen fibers and are distributed in all regions of the articular disc [2].
The internal derangement of the TMJs are the most common non-inflammatory anomalies, being observed even in asymptomatic subjects. This term, internal derangement, differs from what is considered as degeneration because the quality and structure of the tissues are not necessarily altered. It is clear that inflammatory and degenerative TMJ disorders are classified within different groups; however, much coincidence has been found in the clinical course of these two entities because degeneration of articular surfaces can be found with normally located disks and degenerative changes that can be caused by mechanical disk derangement. Because disc displacements have been considered frequent in the young and young adult population, it may suggest a normal congenital anatomical variant. This has been discarded after analyzing MRI images made in the brains of infants from 2 to 5 years who reflected, when observing the TMJs, that the disc occupied a normal position, concluding that the disc displacements are an acquired condition. Therefore, the Magnetic Resonance (MRI) is the best imaging study to evaluate the different elements of the TMJ, and its great contribution is the observation of the situation and normal shape of the joint disk; especially in joint derangements where normal patterns of motion are altered, and where the function of the articular disc is greatly involved [1].
Helms and Kaplan, mentioned by Gökalp et al., state that in the context of MRI, in order to orient ourselves towards a normal disk position or relation with the mandibular head, the image of the posterior band of the disk, with the bilaminar zone, produces a hypointense zone that is located vertically on the mandibular head; and that under physiological conditions, the condyle and the disc relate in that zone that we could call 12 o’ clock zone, considering normal a variation of ±10°. Disc displacements with angles greater than 10° are described as anterior and those with less than 10°, as posterior [3] (Fig. 1).
Fig. 1a), b) Position 12 o’clock. Disk ratio (posterior band junction with bilaminar zone) with mandibular condyle with deviation of ±10°; c) anterior displacement of the disc; d) posterior displacement of the disc [3]
![a), b) Position 12 o’clock. Disk ratio (posterior band junction with bilaminar zone) with mandibular condyle with deviation of ±10°; c) anterior displacement of the disc; d) posterior displacement of the disc [3]](https://static-01.extrica.com/articles/22794/22794-img1.jpg)
Larheim states that according to Kertens the disc in its relation with the condyle, in close-mouth position or maximum intercuspation, can move in three different directions depending on the spatial section it occupies, being normal when the disc occupies the lateral, central and medial section of the mandibular head; partial displacement when the disc is normally located in 2 sections and is displaced in another (disc rotation), and full displacement when the disc is outside all sections [4].
A great contribution of the MRI has been the observation of the situation and shape of the articular disc, in sagittal cuts, which can undergo changes, not only in its relation with the mandibular head and the articular eminence of the temporal, but also in its anatomical configuration and where such distortion can affect the functional conditions of the mandible. Within these forms we find: Biplane when it has an even thickness; Biconvex when its upper and lower surface are convex; Folded when it has doubles in its center and Hemiconvex, when its upper surface is concave and the lower is convex [5] (Fig. 2).
According to the diagnostic criteria for clinical and research applications of temporomandibular disorders, the consensus of experts (RDC/TMD) places internal derangement on the so-called Axis I, which may or may not be accompanied by symptoms, such as pain, functional limitation and noise; and where, although the data identifies the need for imaging to obtain a definitive TMJ-related diagnosis, imaging should not be used routinely, but rather considered when it is important for a patient or investigation [6].
In joint disorders where there are postural alterations between the disc and the condylar head, 80 % to 90 % of cases may be symptomatic, although in a smaller proportion they may also be present in asymptomatic cases (34 %). Hence the importance of supplementing with imaging studies is of great value not only for a successful diagnosis but also for a correct treatment approach [7].
Fig. 2Articular disc configuration classification according to Murakami et al. [5]
![Articular disc configuration classification according to Murakami et al. [5]](https://static-01.extrica.com/articles/22794/22794-img2.jpg)
Over the years, there has been consensus on a conservative approach, as the first line of treatment, in symptomatic disorders of the TMJ; which involves nonsteroidal anti-inflammatory drugs, muscle relaxants, oral appliances, home care, and cognitive behavioral information programs. The focus on oral appliances is that they stabilize or reposition the intermaxillary occlusal relationships, which generate changes in the patient's occlusal behavior, by inducing awareness of some oral parafunction, thus reducing the possibility of further wear, chipping or cracking of the teeth. The theory behind the use of these appliance is to shift the mandibular head to a more advanced position and to allow the recapture of the displaced disc; often used in patients with painful clicks and intermittent locking [1].
Treatments with Jaw Functional Orthopedics (JFO) have been used both in the ontogenetic and post-ontogenetic periods of the individual; its objective is based on removing undesirable interferences during the growth and physiological development of the structures of the stomatognathic system (SS). Such treatments create new postural reflexes, generating another mandibular dynamics that produces and maintains the balance of the entire system. The occlusal plane, as part of the SS, is considered a meeting field of antagonistic teeth that reflects the adaptations to the information given by the neuromuscular activity, controlling the final stop of the masticatory cycle [8], hence its compensations such as the modification of its shape, depending on the chewing activity. In addition, of the conditions that have to do with the occlusal plane, there is a parallelism of reciprocal effects within the periodontium, as in TMJs [9]. In this sense, the changes in the situation of the occlusal plane have an influence on the relationships and dynamics in the structures of the TMJs [10]. Therefore, JFO therapy could be a good option for the treatment of internal disorders of the TMJs.
2. Clinical case
This study presents the case of a 15-year-old male patient who reports very occasional mouth opening locking when getting up in the morning and joint noise on the left side, totally asymptomatic. Facial asymmetry with mandibular deviation to the right side. From the occlusal point of view, it presents overbite and tooth alteration in number and shape (absence of 12, microdontia of 22, transposition of 13 in position of 12 and retention of 53) (Fig. 3).
Fig. 3a) Frontal facial view, asymmetry towards the right side, b) the diastema in the smile of the patient in anterosuperior area can be observed due to dental anomaly of shape and number, c) and d) characteristics of the obtuse labial naso angle is observed, e) Occlusal view: Note the permanence of the right upper temporal canine, f) location of the permanent canine instead of the right lateral incisor, g) abnormal shape of the left lateral incisor
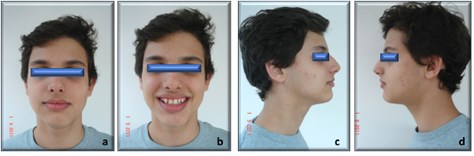

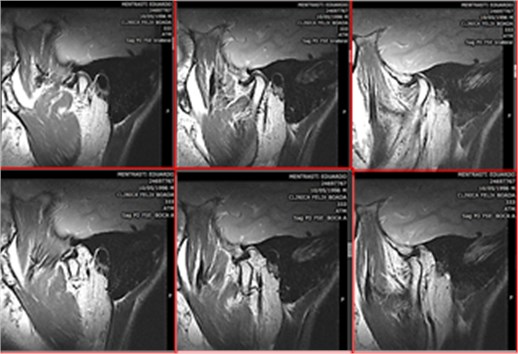
Fig. 4Magnetic Resonance Image of the right TMJ, in a closed mouth position (upper image) Anterior displacement of the disc. (lower image) Open mouth disc displacement without recapture. Even folded type disc deformation is observed in the middle
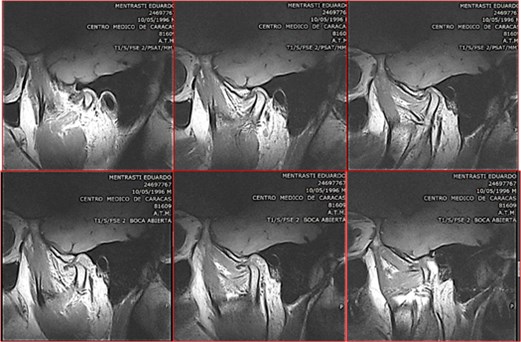
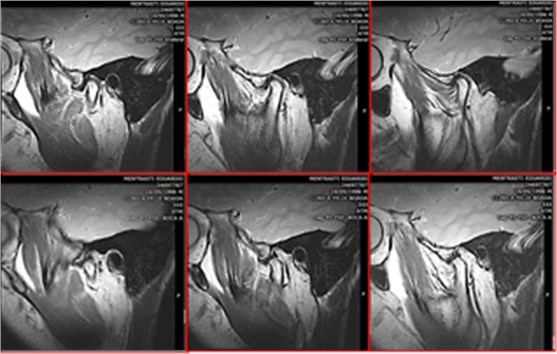
Fig. 5Magnetic Resonance Image sagittal section of the left TMJ, (upper image) mouth closed anterior displacement of the disc; (lower image) Mouth open, disc displacement with reduction. The disc is recaptured during the mouth opening movement
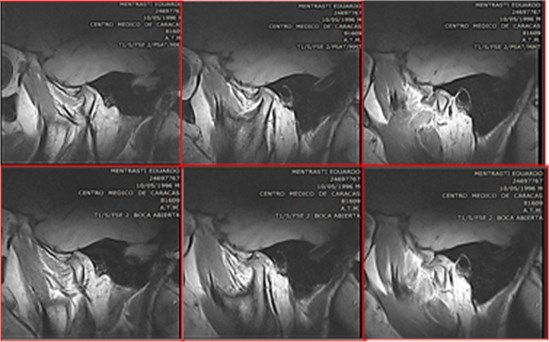
Thanks to the initial MR image of his Temporomandibular Joints, he was diagnosed: in the sagittal plane, anterior displacement of the disc in the closed mouth position, both in the right and left TMJ. In open mouth, disc displacement without reduction in the right temporomandibular joint (Fig. 4), with disc deformation and in the left TMJ anterior disc displacement with recapture (Fig. 5).
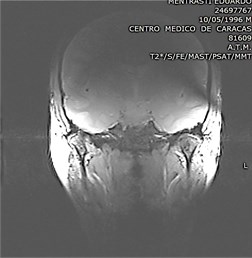
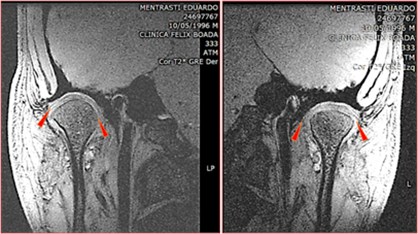
According to the coronal cuts, medial displacement of the right and left disc was found, being more noticeable the disc on the right side Fig. 6.
Fig. 6Coronal section Magnetic Resonance Image, in closed mouth position. Medial disc displacement. The right TMJ is more evident than the left
Planas Indirect composite Tracks were indicated as treatment; (Fig. 7) this particular type of FOA (functional orthopedic appliance) are bioplastic devices that allow partial freedom to the mandibular region and its movement. Therefore, if it’s the case, it allows to reach a position of change of the therapeutic posture, in other words, enables the change of mandibular posture with the respective incisive contact in a determined area. Furthermore, understanding that in cases where the incisive contact is not correct, the vertical dimensions is low, which prevents the complete eruption of the posterior teeth, therefore, resulting in a change in mandibular posture that can also be reflected in the situation of TMJs [8], [9]. When changes in mandibular posture are required in the posteroanterior direction, the respective anatomy of the patient can give references to achieve this; when the vertical sense is considered, it must be proportional and compensatory to the incisive contact in the determined area. This allows for a better and faster response to the treatment.
Fig. 7Planas’ Indirect Composite Tracks. Note the change in posture achieved with the appliances

After 1 year of treatment, the case was reassessed, both from the clinical and imaging point of view with magnetic resonance imaging. Clinically, improvements can be observed, in the occlusal plane the overbite decreased (Fig. 8) and with better functional conditions. Changes were also observed in the mandibular head-disc ratio.
The MRI in the sagittal plane at one year of treatment, in a closed mouth situation, the right TMJ closed, shows anterior displacement of the disc, being recaptured during the initial phase of mouth opening (Fig. 9), improving the joint dynamics. Changes in disk configuration were also observed towards normal patterns.
Fig. 8Occlusal changes obtained with Planas’ indirect composite tracks. JOF treatment
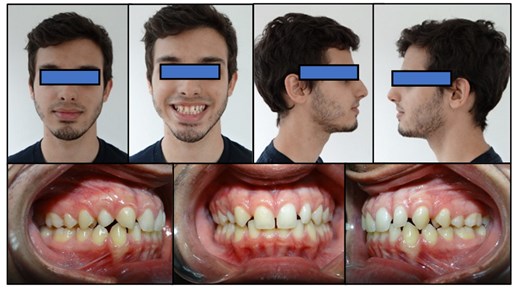
Fig. 9Right temporomandibular joint. (upper image) mouth closed, with anterior disc displacement (lower image) in mouth opening recapture of the disc during movement, without shape alteration
At the level of the left TMJ, the position of the disc in the closed mouth position is observed within normal parameters (12 o' clock), disc positioned on the mandibular head and in the open mouth, translation of the mandibular head- disc complex on the articular eminence of the temporal bone (Fig. 10).
Fig. 10Left temporomandibular joint after treatment with functional orthopedics of the jaws. (upper image) Closed mouth (lower image) Open mouth
From a coronal view, there were also changes in the disc-mandibular head relation; there is a relationship with the disc located on the entire extension of the mandibular head Fig. 11.
Fig. 11View of coronal cuts the disc is located on the condylar head, after treatment
3. Discussion
Magnetic resonance imaging (MRI) is the most effective test for the diagnosis of pathologies affecting TMJ, as it provides anatomical and functional images of hard and soft tissues, especially the joint disk. The internal disorders of the TMJs are the most common non-inflammatory anomalies, not considered degenerative because the quality and structure of the tissues are not necessarily altered [1, 5, 11].
The possibility of analyzing the TMJs in different spatial planes has made it possible to establish suggestions on the ideal position of the disc with respect to the mandibular head, as well as disc shaped distortions that can be interpreted as a response to loads that may affect the functional conditions of the jaw [3-5].
The RDC/TMD consensus places the internal disorders of the TMJs within the so-called Axis I, and although they may or may not come accompanied by symptoms, such as pain, functional limitation and noise; consider that the TMJ imaging studies should not be used routinely [6]. However, although between 80 and 90 % of cases with postural alterations between disc and mandibular head may present symptoms, there is a low proportion of asymptomatic cases (34 %). Therefore, it would be ideal to complement a diagnosis with imaging studies of the TMJs to guide a good treatment approach [7].
Conservative treatment is the choice for these clinical entities, consisting of drugs, oral appliances, home care and cognitive behavior information programs. The use of oral appliances has also been indicated that aim to stabilize or reposition the intermaxillary relationships, in order to look for changes in the occlusal behavior of the patient and induce awareness of some oral parafunction. In fact, this appliance suggests moving the mandibular head to a more advanced position and thus allowing the recapture of the displaced disc [1].
The Jaw Functional Orthopedics (JFO) creates new postural reflexes by changing the mandibular dynamics, a factor that produces and maintains the balance of the entire stomatognathic system (SS). Orthopedic devices, by modifying the functionality of the entire SS, stimulate responses at the occlusal plane level as a reflection of adaptation to the information given by muscular work and masticatory function, and there is also a parallelism of reciprocal effects between the periodontium, TMJs and neuromuscular activity [8-10]. Thus, the change in mandibular posture and the adaptations of the occlusal plane influence postural and functional changes of the TMJs.
4. Conclusions
Magnetic resonance imaging is the ideal technique for the study of TMJ arthropathies as it provides anatomical and functional images of the hard and soft tissues, especially of the articular disc in a static or dynamic situation. This technique allows us to describe the situation of the disc in the closed and open mouth, to interpret the loads that occur within the TMJs and how they influence mandibular movements. Temporomandibular disorders may or may not present symptoms, and it is precisely with the latter that we must have careful clinical criteria to indicate imaging studies such as MRI; in order to observe and analyze how the articular disc behaves with the other structures that make up the TMJ, to establish a correct diagnosis that leads us to the best treatment, despite the absence of symptoms.
The JFO represents a treatment option for joint dysfunctions or disorders; the therapeutic and mandibular posture change modifies SS functional patterns, within physiological limits, which stimulate adaptive responses reflected in the situation of the occlusal plane, neuromuscular activity and TMJs. Therefore, it is possible to partially or totally correct the disorders between the articular disc and the mandibular head, perhaps depending on how early the diagnosis and treatment are made, hence the importance of MRI.
References
-
F. Molinari, P. F. Manicone, L. Raffaelli, R. Raffaelli, T. Pirronti, and L. Bonomo, “Temporomandibular joint soft-tissue pathology, I: disc abnormalities,” Seminars in Ultrasound, CT and MRI, Vol. 28, No. 3, pp. 192–204, Jun. 2007, https://doi.org/10.1053/j.sult.2007.02.004
-
Alejandrina Millón Cruz, “Empleo de la resonancia magnética (RM) en el diagnóstico de perforaciones discales de la articulación temporomandibular: correlación clínico-radiológica,” Ph.D. Thesis, Universidad Complutense de Madrid, 2021.
-
H. Gokalp, “The changes in temporomandibular joint disc position and configuration in early orthognathic treatment: a magnetic resonance imaging evaluation,” The European Journal of Orthodontics, Vol. 22, No. 3, pp. 217–224, Jun. 2000, https://doi.org/10.1093/ejo/22.3.217
-
T. A. Larheim, “Role of magnetic resonance imaging in the clinical diagnosis of the temporomandibular joint,” Cells Tissues Organs, Vol. 180, No. 1, pp. 6–21, 2005, https://doi.org/10.1159/000086194
-
S. Murakami, A. Takahashi, H. Nishiyama, M. Fujishita, and H. Fuchihata, “Magnetic resonance evaluation of the temporomandibular joint disc position and configuration,” Dentomaxillofacial Radiology, Vol. 22, No. 4, pp. 205–207, Nov. 1993, https://doi.org/10.1259/dmfr.22.4.8181648
-
E. Schiffman et al., “Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: recommendations of the international RDC/TMD Consortium network and orofacial pain special interest group,” Journal of Oral and Facial Pain and Headache, Vol. 28, No. 1, pp. 6–27, Jan. 2014, https://doi.org/10.11607/jop.1151
-
D. González-Ballester, R. González-García, A. García Nogales, C. Moreno García, and F. Monje Gil, “¿Es el desplazamiento discal sinónimo de patología articular temporomandibular? Correlación clínico-radiológica y prevalencia de trastornos internos en sujetos voluntarios asintomáticos.,” Revista Española de Cirugía Oral y Maxilofacial, Vol. 42, No. 3, pp. 97–106, 2020, https://doi.org/10.20986/recom.2020.1133/2020
-
W. Simões, “Modulation of occlusal plane during puberty,” Journal of Clinical Pediatric Dentistry, Vol. 19, No. 4, pp. 259–268, 1995.
-
W. Simões, Ortopedia funcional de los Maxilares Vista a Través de la Rehabilitación Neuro-oclusal. Caracas: Ediciones Isaro, 2004.
-
E. Zambrano, A. Y. Hernández, and A. Morón, “Influência do plano oclusal naarticulaҫão temporomandibular,” Revista Internacional de Ortopedia Funcional, Vol. 2, No. 9, pp. 682–701, 2006.
-
G. Concha, “Imágenes por resonancia magnética de la articulación temporomandibular,” Revista HCUCh, Vol. 18, pp. 121–30, 2007.
About this article
The authors have not disclosed any funding.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
The authors declare that they have no conflict of interest.
Permit to perform biomedical investigation was granted by Sandra de Mentrasti, to Grupo Odontologico Zambrano under the case number 5087, on December 27th, 2010. Participants provided written consent before starting the treatment.
