Abstract
The treatment of impacted teeth requires an interdisciplinary approach, in which early diagnosis avoids later complications. The frequency of canine retention, especially of the lower canines, has a 0.22 % average in the general population. Case information: A 9.1-year-old patient presented Lepto/Lepto, Lepto; distocclusion due to retrognathism and maxillary protrusion with left condylar asymmetry and preferential chewing on the right side. The patient also presented a structural open bite (Lower Go 78°) hyper-divergence level 4; severe crowding with complete lack of space for tooth 33, and alteration of the eruption corridor of tooth 43. Objective: Stimulate jaw growth to correct distocclusion, stimulate transversal development to gain space and eliminate crowding, and exercise traction on the lower right canine to position it correctly and correct asymmetry. Methods: A series of functional orthopedics devices were used. A Standard Bimler during the first 6 months, subsequently, Simões Network 1 (SN1) to conquer space and initiate traction, followed by the use of an SN11 to correct asymmetry with contra attachment for de-rotation and a lingual S spring. Results: It was possible to obtain incisive contact and align the anteroinferior segment, full space was obtained for tooth 33. Traction of tooth 43 was achieved and thus asymmetry was controlled. Conclusions: Functional orthopedic techniques are an effective form of dental traction that favors treatment from different perspectives. On one hand, it allows to gain space to eliminate crowding. On the other hand, it does not affect neighboring or antagonist teeth because the anchorage is not on the teeth, and it is not necessary to place intraosseous mini-implants. Also, an adequate surgical and functional orthopedic procedure makes it possible to traction the impacted teeth, orienting them to erupt and occupy the correct position in the dental arch.
Highlights
- In cases of lower canines with the tendency to transmigrate, an early diagnosis plus jaw functional orthopedics is possible to treat it.
- Correct the eruption corridor and perform traction of the lower with anchorage typical of functional orthopedic techniques.
- Unlike conventional orthodontic techniques, with the proposed technique, it is possible to correct crowding and create space for the canines without the need for permanent tooth extractions.
- In addition, control of vertical and transverse growth is achieved, as well as the alignment and inclination of the teeth.
1. Introduction
Dental eruption is influenced by various factors, which makes it a very complex process that may suffer in the presence of malocclusion. One of the most common eruption alterations is dentary impaction. Dentary impaction should be understood as the total or partial lack of a tooth’s eruption. Said tooth is covered by soft tissue or bone, which makes its future eruption unlikely [1]. Canine impaction is the second most common dentary impaction, after that of the third molars [2]. Canine impaction varies in frequency depending on the population studied. The incidence of maxillary canine impaction is 1 to 3 %, [3] while the incidence of impaction on mandibular canines is considered low 0.22 % [4]. Meanwhile, in 2009, an incidence of mandibular canine impaction of 1.29 % was reported [5] nonetheless, there is very little literature available that deals with the treatment of cases of mandibular canine impaction.
Additionally, teeth that migrate in an intra-osseous manner have been referred to using the term transmigration, which, although rare, is found more often in mandibular canines [6]. Transmigration usually occurs in a mesial direction, which results in migration through the mandibular symphysis towards the opposing side [7]. Mupparapu et al., have suggested a classification of transmigration of mandibular canines in order to have a better understanding of this phenomenon, as well as a more appropriate communication and more adequate treatment [8]. The objective of this work is to contribute with the report of a case of this kind of anomaly, and to report the therapeutic methods used.
2. Clinical case or presentation of the case.
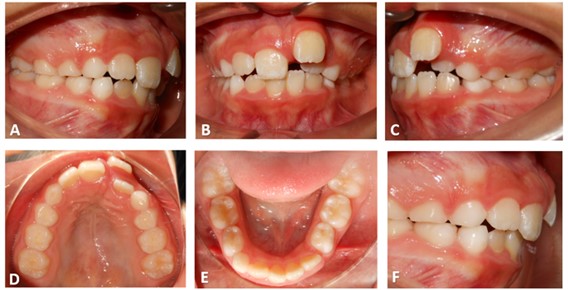
A 9.1-year-old male patient, from the city of Queretaro, Mexico, was admitted to the Jaw Functional Orthopedics clinic due to the malposition of his anterior teeth. The patient did not have any pathological precedents. The patient had a Leptoprosopo biotype, a convex profile, and clinical exploration revealed a difference in size and shape of the patient’s hemimandibles, as well as lack of labial closure due to hypertonicity of the chin (Fig. 1). An intraoral exploration revealed severe crowding in the anterior region, both upper and lower; and a complete lack of space for tooth 33 (Fig. 2).
Fig. 1In this image the difference in shape of the hemimandibles can be seen: a) note the dryness of the lips due to the lack of closure, b) upon forcing closure of the lips, the chin’s hypertonicity becomes visible
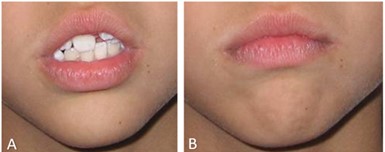
Fig. 2Intra-oral photographs in which the beginning of the treatment is depicted: a) note the flat occlusal plain with physiological wear, b) the upper left incisor protrudes and is superimposed upon the lateral incisor, c) complete lack of space for the inferior canine, d) superior arcade lacking transversal development, e) non-symmetric shape of the arcade due to lack of development, f) note the protrusion of the superior incisors
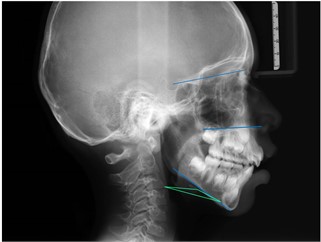
To diagnose the patient, panoramic and lateral cranial x-rays were taken. In the panoramic radiograph, it was performed Simões’ symmetry analysis, and this allowed us to diagnose structural asymmetry, a higher condyle, and a mandibular angle on the left side. Once the Planas’ functional masticatory angles analysis was applied, the presence of a right-side masticatory preference was detected. This compound asymmetry renders treatment more complex. The dental analysis revealed an altered eruption corridor of tooth 43, which, according to its position mesioangularly across the midline within the jaw bone, lingual or labial to anterior teeth that according to Mupparapu’s classification, corresponds to type 1. With regards to tooth 33, its space was mined by the eruption of tooth 32, which left tooth 33 without the necessary room to erupt. On the upper maxillary, a severe lack of space to house the permanent teeth was also found (Fig. 3). As to the lateral cranial x-ray, a Bimler analysis was performed, which revealed the presence of a type II retrognathism and maxillary protrusion. The patient also presented a structural open bite and level 4 hyper-divergence, in which the hyperextension of the head compensates for the jaw’s low position, which results in an alteration of the relation between hyoids, the mandible, and the services [9] (Fig. 4). The patient’s prognostic was reached with the support of a Petrovic cephalometric analysis, which revealed a P2DOB rotational group, which indicates a posterior condylar growth rotation, a decreased mandibular growth potential in comparison to the maxillary, a distal sagittal relation of the mandible with a tendency to an open bite with a low tissular response. Based on this and the clinical and cephalometric characteristics of the patient, we could foresee that the treatment would be complicated, as it required paying attention to many different aspects such as asymmetry, lack of space, and the correction of the position of the mandibular canine.
Fig. 3Panoramic x-ray in which the asymmetry and the position of tooth 43, which was classified as a type 1 canine transmigration on Mupparapu’s scale, can be observed

Fig. 4This x-ray shows the divergent horizontal plains, as well as the inverted hyoid triangle
3. Therapeutic intervention and treatment results
The treatment’s objectives were to stimulate sagittal growth of the mandible and, at the same time, stimulate transversal development in order to gain space and correct dental crowding. Treatment began with the placement of a standard Bimler functional orthopedic appliance (Fig. 5(a, b)). The patient was instructed to activate the appliance with a ¼ turn of the screw every 8 days, and the patient attended a check-up every 30 days to do the correct activation of the different parts of the orthopedic appliance. After five months, the crowding in the anterior upper sector surrounding tooth 22 showed some relief, and the protrusion of tooth 21 improved. In the inferior dental arch, an increase in the space to house tooth 33 (Fig. 6(a)) was evidenced. Prints were taken to make a Simões Network 1 (SN1) appliance, [10] with the goal of further stimulating the sagittal growth of the mandible and transversally stimulating the maxillaries. The patient was instructed to activate the appliances by turning the upper and lower screws ¼ of a turn every 8 days, and the patient attended medical check-ups at the clinic every 30 days to review and verify the activation of all the parts of the new appliance.
Fig. 5Standard Bimler Appliance used at the beginning of the treatment. At a later stage, an SN1 was used since in addition to its attributes to stimulate development at the sagittal and transversal sense, it favors anchorage for traction of the lower tooth. Subsequently, it was placed an SN11 with an accessory to correct the canine rotation
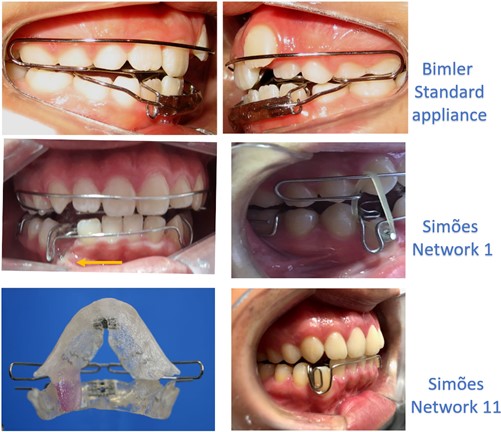
Fig. 6a) At age 9.6 years, the increase of the patient’s space for tooth 33 and the alignment of the anterior-upper segment can be observed; b) At age 10, the patient is remitted to the surgeon to bind the canine and initiate traction. Note how the middle line is deviated; c) The cut in the wire that was applying traction to tooth 43 can be observed. The complete space for tooth 33 is also visible, but this tooth is in canine class II; d) Eruption of tooth 43 began with a rotation. On the left side, the canines are already oriented into class I; e) The improved position of tooth 43 and the middle line are visible. On the left side, the upper and lower canines have erupted with a class I for canines and molars

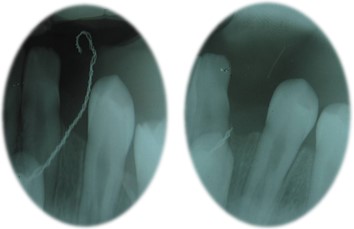
After six months of using the SN1, the sequential extraction of the first decidual upper and lower molars was performed with the goal of improving the eruption corridors of the permanent canines. The extraction was performed following Simões’ concept of sequential extraction.[11] The patient was remitted to the maxillofacial surgeon to bind tooth 43. By this point, the full space could be seen, and the eruption of tooth 33 began (Fig. 6(b)). The patient continued to use the SN1 appliance and anchorage accessories were placed to create traction for tooth 43. First, distal horizontal traction was applied to disincline tooth 43 (Fig. 5(c)). Later, the vector of the traction was modified to a vertical axis, with anchorage on the vestibular arch (Fig. 5(d)). A 1.5 oz (equivalent to 42.5 grams) weight was used, and the patient was permanently asked whether there was any pain or discomfort. Ten months after beginning to apply traction to tooth 43 the wire which was applying traction to the canine was cut. An x-ray of the area showed that the tooth was correctly oriented along its eruption corridor, so no further surgical procedures were required (Fig. 7). Later a Simões Network 11 (SN11) was used to control and correct the asymmetry with a vertical fin on the left side to orient the mandible towards the middle line. Finally, some Planas Simple Indirect Tracs were placed with the goal of rendering the mandibular movements functional and finalizing the process of equilibrating the occlusal plane.
Fig. 7It is observed that the wire with which the canine was being pulled is cut, for which an x-ray was taken in which it can be seen how tooth 43 had become aligned with its eruption corridor. For this reason, it was not necessary to perform a surgical procedure again
4. Discussion
Retention is the term used to describe when a permanent tooth hasn’t erupted within a period of a full year after the normal age of eruption [12]. Retention is considered relatively rare, except for the third molars and the upper canines, for this reason, retention of the mandibular canines, since it has a relatively low incidence [13], can be one of the reasons for the lack of literature dealing with the subject. Transmigration is the term used to describe the migration of a tooth through the mandible’s middle line [14]. The etiology of transmigration of the mandibular canines is not clear [15], and many cases have been reported in which there is no associated pathology [16]. In the meantime, it has been observed that there are certain characteristics that are present in cases of impaction and transmigration of the mandibular canines, and upon which many authors coincide, such as the presence of odontomas and cysts, [17] which did not occur in the present case report. It has been observed that type II malocclusion of the anterior-inferior facial height may be a predisposing factor; [18] these characteristics coincide with the present case report, in which the patient evidenced type II hyper-divergence with a gonial angle of less than 78°. On top of the aforementioned factors, Vichi and Franchi have emphasized since 1991 that observed characteristics should be taken into account in order to make an early diagnosis of a patient with transmigration and mandibular canine impaction. Among the most important points is evidence of a canine that hasn’t erupted and can be felt in a mesial position on the labial groove, an enlarged symphysis mentalis area can be seen, and the inferior incisors are inclined [19]. In the reported case an enlargement of the symphysis mentalis of the right side was found, which further accentuated the facial asymmetry. Additionally, determinant genetic signs were found [20]. The crowding of the teeth is another aspect of the discussion since some authors haven’t found crowding to be a factor associated with transmigration [16] and have even shown that bilateral migration of the mandibular canines can be present even when there is enough room for their eruption [21]. But Holla, Saify, and Parashar consider that it may be a factor related to etiology [18]. In the same way, it is known that it is probable that a difference in arch length may cause impaction [22]. In the present case report, there were no spaces for functional development and the teeth had moved to the left due to the premature loss of the decidual canine on the left side. Although the theories identify the etiology of this phenomenon, the displacement of the dental plate to an abnormal position in the early stages of development can be considered a cause for teeth deviating into abnormal eruption corridors.[23] A study was published recently in which febrile diseases and endocrine deficiencies were also considered etiological factors, and which suggested that the size of the space available to house teeth should also be considered [24]; we coincide with this last point since in the present case we found a large disparity between the dentary material and the available space. We believe that, depending on the patient’s age and the moment at which the diagnosis is made, the retained mandibular canine (as in this case) may become a case of transmigration when it is subjected to certain factors such as its inclination [25] since this phenomenon can be found at an early age during which a mixed denture is present, and may take place during a period of many years [6]. In the present case, the patient was treated at a young age at which a retained tooth couldn’t be diagnosed since its active eruption period wasn’t over, nonetheless, it was evident that the tooth wasn’t on a correct eruption corridor. We agree with Hudson, [26] the claim that the diagnosis must be made at an early age, otherwise, given the characteristics present in the patient, the canine could have transmigrated.
Even when few cases of dentary impaction and mandibular canine transmigration have been reported, several possibilities for treating such cases have been suggested, among which are orthodontic treatment, surgical intervention, transplants, and functional orthopedics. On the other hand, several authors have reported the need to extract a retained tooth or one that has transmigrated. In a retrospective study, 88 patients were analyzed with a total of 94 mandibular canines, of which half of those that were impacted but hadn’t transmigrated were fixed orthodontically, and half of those that had transmigrated were surgically removed [27]. Another study in which the authors studied 102 patients with a total of 118 impacted canines, 24 of which were mandibular canines, resulted in 4 surgical extractions, 9 trans-alveolar transplants, 8 corrected with orthodontic traction after an initial surgical intervention, 3 spontaneous eruptions once the necessary space had been acquired, and no cases of treatment using removable appliances as well as no cases of decidual canine extraction [28]. We coincide with van der Linden and Singh regarding the extraction of certain decidual teeth which comprise interception at the correct time [29], [30]; but, on the other hand, we coincide with Naoumova and colleagues in that the extraction of decidual canines is the variable which most affects spontaneous eruption of canines [31]. In our revision of published articles, we didn’t find documented cases of mandibular canines treated with functional orthopedics. One case of an impacted right mandibular canine was reported, very similar to the case presented in this report, in which therapeutic orthodontic extraction of the superior pre-molars and extraction through agenesia of the second inferior pre-molars was used [32]. Although in the present case, no permanent teeth were extracted despite the patient’s extreme lack of space for housing all the permanent teeth, on top of the proclination of the upper incisors; we coincide with the authors of the beforementioned case in the times employed during the different phases of the treatment.
It is important to stress the importance of the patient’s strict adherence to the treatment as a large part of the results depends on this. In the present case, despite the prognostic being unfavorable, not only because of the problem with tooth 43 but also because of the gravity of the lack of space and the evident hyper-divergence, the results proved the efficacy of the treatment, as all the objectives were achieved. Nonetheless, obtaining the correct positioning of tooth 43, correcting the middle line and the ortho-inclination of the lower incisors are still pending.
5. Conclusions
It can be concluded that functional orthopedic techniques are an effective way to treat impacted mandibular canines, as they favor treatment from different perspectives. The therapeutical methods used in this case promoted the mandible’s sagittal development, and, at the same time, produced transversal development to correct the lack of space for permanent teeth. The functional orthopedic techniques contain their own anchorage and thus don’t affect neighboring or antagonist teeth which, as they have nothing on them, can erupt at the adequate age, thus enabling early treatment. Also, there is no need for intra-osseous implants. An adequate orthopedic and surgical procedure may traction the impacted teeth orienting them to occupy their correct position. On the other hand, the patient’s strict adherence to the treatment is fundamental in order to obtain favorable results in a time comparable to or lower than that of other techniques.
References
-
D. P. Singh, A. K. Garg, L. Singla, and T. Das, “Closed eruption of impacted mandibular canine,” Orthodontic Waves, Vol. 70, No. 3, pp. 108–118, Sep. 2011, https://doi.org/10.1016/j.odw.2011.05.002
-
M. E. Montes-Díaz, A. Martínez-González, R. Arriazu-Navarro, A. Alvarado-Lorenzo, N. E. Gallardo-López, and R. Ortega-Aranegui, “Skeletal and dental morphological characteristics of the maxillary in patients with impacted canines using cone beam computed tomography: a retrospective clinical study,” Journal of Personalized Medicine, Vol. 12, No. 1, p. 96, Jan. 2022, https://doi.org/10.3390/jpm12010096
-
S. E. Bishara, “Clinical management of impactedmaxillary canines,” Seminars in Orthodontics, Vol. 4, No. 2, pp. 87–98, Jun. 1998, https://doi.org/10.1016/s1073-8746(98)80006-6
-
Cruz Rm, “Orthodontic traction of impacted canines: Concepts and clinical application.,” Dental Press Journal of Orthodontics, Vol. 24, No. 1, pp. 74–87, 2019, https://doi.org/10.1590/2177-6709.24.1.074-087
-
T. S. Yavuz Ms, Aras Mh, and Büyükkurt Mc, “Impacted mandibular canines,” Journal of Contemporary Dental Practice, Vol. 8, No. 7, pp. 78–85, 2007.
-
N. Umashree, A. Kumar, and T. Nagaraj, “Transmigration of mandibular canines,” Case Reports in Dentistry, Vol. 2013, pp. 1–7, 2013, https://doi.org/10.1155/2013/697671
-
V. M. Tarsariya, C. Jayam, Y. S. Parmar, and A. Bandlapalli, “Unusual intrabony transmigration of mandibular canine: Case series (report of 4 cases),” BMJ Case Reports, Vol. 2015, p. bcr2014205398, Sep. 2015, https://doi.org/10.1136/bcr-2014-205398
-
Muralidhar Mupparapu, Ajit Auluck, Setty Suhaz, Keerthilatha M. Pai, and Archna Nagpal, “Patterns of intraosseous transmigration and ectopic eruption of bilaterally transmigrating mandibular canines: radiographic study and proposed classification,” Quintessence International (Berlin, Germany: 1985), Vol. 38, No. 10, pp. 821–828, 2007.
-
W. A. Simoes, “Maxillary functional orthopedics,” (in Italiano), Trestina, PG Italia, 2010.
-
W. A. Simoes, “Insights into maxillary and mandibular growth for a better practice,” The Journal of Clinical Pediatric Dentistry, Vol. 21, No. 1, pp. 1–7, 1996.
-
W. A. Simoes, “Ortopedia funcional de los maxilares,” Wilma Alexandre Simões-Artes Médicas, São Paulo, 2004.
-
Daniel Torres-Lagares, Rafael Flores-Ruiz, Pedro Infante-Cossío, Manuel García-Calderón, and José Luis Gutiérrez-Pérez, “Transmigration of impacted lower canine. Case report and review of literature,” Medicina Oral, Patologia Oral Y Cirugia Bucal, Vol. 11, No. 2, pp. E171–E174, Mar. 2006.
-
A. Almarhoumi, Y. Okashah, M. Alrehaili, and K. Alrehaili, “Frequency and pattern of impacted Canines in Al-Madinah, Saudi Arabia: A cross-sectional radiographic study,” Journal of Orthodontic Science, Vol. 11, No. 1, p. 15, 2022, https://doi.org/10.4103/jos.jos_188_21
-
P. Shanmuhasuntharam and L. C. Boon, “Transmigration of permanent mandibular canines. Case report,” Australian Dental Journal, Vol. 36, No. 3, pp. 209–213, Jun. 1991, https://doi.org/10.1111/j.1834-7819.1991.tb04705.x
-
S. E. Camilleri S., “Transmigration of mandibular canines--a review of the literature and a report of five cases.,” The Angle Orthodontist, Vol. 73, No. 6, pp. 753–62, 2003, https://doi.org/10.1043/0003-3219(2003)073
-
P. Plakwicz et al., “The retrospective study of 93 patients with transmigration of mandibular canine and a comparative analysis with a control group,” European Journal of Orthodontics, Vol. 41, No. 4, pp. 390–396, Aug. 2019, https://doi.org/10.1093/ejo/cjy067
-
D. Dalessandri, S. Parrini, R. Rubiano, D. Gallone, and M. Migliorati, “Impacted and transmigrant mandibular canines incidence, aetiology, and treatment: a systematic review,” European Journal of Orthodontics, Vol. 39, No. 2, pp. 161–169, Apr. 2017, https://doi.org/10.1093/ejo/cjw027
-
Anup Holla, Mansoor Saify, and Sandeep Parashar, “Transmigration of impacted mandibular canines and its association with malocclusion and morphology: an analysis of seven cases,” Orthodontics: the art and practice of dentofacial enhancement, Vol. 13, No. 1, pp. 156–165, 2012.
-
M. Vichi and L. Franchi, “The transmigration of the permanent lower canine,” Minerva Stomatologica, Vol. 40, No. 9, pp. 579–589, Sep. 1991.
-
S. Peck, “On the phenomenon of intraosseous migration of nonerupting teeth,” American Journal of Orthodontics and Dentofacial Orthopedics, Vol. 113, No. 5, pp. 515–517, May 1998, https://doi.org/10.1016/s0889-5406(98)70262-8
-
K. M. Shapira Y., “Intrabony migration of impacted teeth.,” The Angle Orthodontist, Vol. 73, No. 6, pp. 738–43, 2003, https://doi.org/10.1043/0003-3219(2003)073
-
H. Al-Zoubi, A. A. Alharbi, D. J. Ferguson, and M. S. Zafar, “Frequency of impacted teeth and categorization of impacted canines: A retrospective radiographic study using orthopantomograms,” European Journal of Dentistry, Vol. 11, No. 1, pp. 117–121, Jan. 2017, https://doi.org/10.4103/ejd.ejd_308_16
-
U. A. Bhullar Mk, Aggarwal I., and Verma R., “Mandibular canine transmigration: report of three cases and literature review,” Journal of International Society of Preventive and Community Dentistry, 2017.
-
A. K. Mohammed, G. Sravani, D. Vallappareddy, A. R. Rao, A. Qureshi, and A. N. Prasad, “Localization of impacted canines – a comparative study of computed tomography and orthopantomography,” Journal of Medicine and Life, Vol. 13, No. 1, pp. 56–63, Jan. 2020, https://doi.org/10.25122/jml-2020-0001
-
Ujwal Kontham, Rakesh Kontham, and Jagruti Mistry, “Transmigration of mandibular canines in siblings: a case report,” Quintessence International (Berlin, Germany: 1985), Vol. 43, No. 1, pp. 45–49, Jan. 2012.
-
A. P. G. Hudson, A. M. P. Harris, and N. Mohamed, “Early identification and management of mandibular canine ectopia,” SADJ: Journal of the South African Dental Association, Vol. 66, No. 10, pp. 462–467, Nov. 2011.
-
M. H. Bertl, C. Frey, K. Bertl, K. Giannis, A. Gahleitner, and G. D. Strbac, “Impacted and transmigrated mandibular canines: an analysis of 3D radiographic imaging data,” Clinical Oral Investigations, Vol. 22, No. 6, pp. 2389–2399, Jul. 2018, https://doi.org/10.1007/s00784-018-2342-0
-
J. Stabryła, P. Plakwicz, K. Kukuła, M. Zadurska, and E. M. Czochrowska, “Comparisons of different treatment methods and their outcomes for impacted maxillary and mandibular canines,” The Journal of the American Dental Association, Vol. 152, No. 11, pp. 919–926, Nov. 2021, https://doi.org/10.1016/j.adaj.2021.05.015
-
H. Singh, T. Mittal, P. Sharma, P. Kapoor, R. K. Maurya, and S. Rastogi, “Interceptive orthodontic management of mandibular lateral incisor-canine transposition using simplified and efficient biomechanical approach: A case report,” International Orthodontics, Vol. 20, No. 4, p. 100690, Dec. 2022, https://doi.org/10.1016/j.ortho.2022.100690
-
F. P. G. M. van der Linden, “Recognizing and preventing disturbances in eruption,” Nederlands Tijdschrift Voor Tandheelkunde, Vol. 121, No. 4, pp. 203–208, Apr. 2014.
-
J. Naoumova, J. Kürol, and H. Kjellberg, “Extraction of the deciduous canine as an interceptive treatment in children with palatally displaced canines-part II: possible predictors of success and cut-off points for a spontaneous eruption,” European Journal of Orthodontics, Vol. 37, No. 2, pp. 219–229, Apr. 2015, https://doi.org/10.1093/ejo/cju102
-
W. Northway, “Orthodontic management of a dental anomaly pattern (DAP) including mandibular canine transmigration: A case report: A challenging treatment but worth it!,” The Angle Orthodontist, Vol. 89, No. 1, pp. 149–162, Jan. 2019, https://doi.org/10.2319/021018-115.1
About this article
The authors have not disclosed any funding.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Aidé Terán: conceptualization, investigation, methodology and fabrication of orthopedics appliances, project administration, resources, supervision, validation, visualization, writing – original draft preparation, writing – review and editing. Ana Lucia Compean: Investigation, methodology and fabrication of orthopedics appliances, software. Karla Itzel Yañez: methodology and fabrication of orthopedics appliances, software. Miguel Lloret: data curation, investigation, methodology and fabrication of orthopedics appliances, project administration, resources, supervision, validation, visualization, writing – original draft preparation, writing – review and editing.
The authors declare that they have no conflict of interest.
The patient gave informed consent at the start of treatment.

