Abstract
Anterior Open Bite (AOB) is a malocclusion for which the choice of a treatment protocol it is challenging. There are some protocols that have been shown to be effective for open bite treatment. The aim of this investigation was to study the behavior of overbite during AOB treatment with Jaw Functional Orthopedics (JFO). The behavior of overbite was studied retrospectively in 17 patients treated in the Specialization Course in (JFO – ABO Muriaé (Muriaé, MG Brazil). Monthly overbite measurements in millimeters were taken with a pachymeter and the data were stored in an individual paper worksheet. Data obtained before functional appliance installation (T0) and after 12-months of treatment (T1) were compared. Wilcoxon non-parametric test for 2 paired samples was use for statical treatment of the data. P= 0.003 for overbite comparison T1-T0. It could be concluded that Functional orthopedic appliance has shown to be an effective tool for treating anterior open bite in the sample studied. Further studies, mainly Randomized Clinical Trials, with larger samples are necessary to confirm this result and to study stability and skeletal behavior in anterior open bite treated with Jaw Functional orthopedics.
1. Introduction
Anterior open bite (AOB) can be a most challenging treatment and there is considerable controversy as regards treatment protocols. According to Rijpstra and Lisson [1] the only agreement among authors is that it is an extremely difficult treatment. Even the definition of anterior open bite is controversial. Todoki et al. [2] added that not only treatment but the retention time required, and stability of results are not completely clear. There is a consensus with regard to the etiology of anterior open bite. Genetic factors associated with parafunctional habits such as finger or pacified sucking, upper air way obstructions that lead to mouth breathing and tongue posture have been recognized as etiological factors [2].
Treatment protocols involve the use of fixed appliances, orthognathic surgery, temporary anchorage devices with mini-screws or mini-plates, aligners, headgears, bite blocks [2-9]. Vela-Hernández et al [7] reported that build-ups on posterior teeth are an efficient tool for AOB treatment in adults, as they act in a similar way to bite blocks by promoting a mandibular rotation. Wang et al [8], in a systematic review, reported that orthognathic surgery was an efficient tool in AOB treatment, but the stability varied according to the surgical protocol used. According to the authors bimaxillary surgery produced more stable results than mandibular or maxillary surgeries alone.
In a systematic review, Santos et al [10] reported that there was insufficient evidence to allow inference to be drawn about the effects of AOB treatment with the functional orthopedic appliances used in the treatment. In the Randomized Clinical Trials (RCT), they identified, and recovered the techniques used by Fränkel, a comparison between fixed and removable palatal crib, chin cap and bonded spurs. They included any type of functional appliance used for AOB treatment such as Fränkel, bionator, Sns, Bimler, Planas in comparison with a no treatment, alternative treatment or wait-list control.
Skeletal anterior open bite should not be treated solely with tooth movement. For instance, when molars are intruded, mandible rotation is expected to achieve the anterior guide in protrusive movement. Orthodontics (that is to say use of brackets and wires) used alone does not treat anterior open bite if it involves a skeletal component. In this case, it is always necessary the use orthopedic procedures. There are several orthopedics procedures that have been proved to be efficient in skeletal open bite treatment such as mini-implants, surgical procedures, extra oral appliances, etc.
The aim of this investigation was to check whether Jaw functional Orthopedics would be an efficient tool to improve the overbite in patients with AOB.
2. Materials and methods
The variation in clinical overbite of 17 patients. treated in different (JFO) courses was followed-up monthly for 12 months. A Term of Free and Informed Consent was prepared and signed by all patients or their legal guardians.
The overbite was measured with analogic pachymeters in the following way if there was no trespass of incisors the distance between the incisal borders of the mandibular and the maxillary incisor where the distance was greater was measured and received a minus (-) sign. If there was trespass of the incisors the incisal border of the maxillary incisor was marked on the vestibular surface of the mandibular incisor by using a 0.7 pencil and the distance between the mark and the incisal border of the mandibular incisor was measured. The operators were previously calibrated on dental casts with and without incisor trespass, until they reached the same measurement of the overbite in both situations.
Monthly measurements were made at each clinical appointment before activation of the Functional Orthopedic Appliance (FOA) to follow-up the variation in overbite for treatment reasons, and the data were registered on an individual paper worksheet for each patient. Neither the operator nor patient knew about the destination of the data obtained. The measurements were obtained in millimeters (mm), then the data was collected from the patient’s measurement worksheet, submitted to statistical analysis and was recorded in Tables 1 and 2 and Fig. 1.
Fig. 1Overbite without incisor trespass, measured with a pachymeter

The Sample was composed of 17 patients 9 females and 8 males with age ranging from 7 to 34 years at the day of installation of the FOA, the mean age is 14 years. Twelve patients were treated with SN3 (Simões Network 3 –Lower Winglets Model), three patients treated with SN6 (Simões Network 6 – Special Pad Model) and 2 patients treated with SN2 (Simões Network 2 – Tongue Maintainer Model) [11] Constructed according to Santiago Jr and Santiago instructions [12]. The initial overbite ranging from – 10 mm to 0 mm Table 1.
For the statistical analysis, the SPSS 11.0 was used. The assumption of normality was verified through the test of Shapiro-Wilk. Since the variable overbite did not present normal distribution (P<0.05) to compare overbite T0 and overbite T1 Wilcoxon non-parametric test was used for 2 paired samples. The level of significance was P< 0.05.
Table 1Description of Sample and overbite behavior. T0 overbite measurement in mm before treatment, T1 overbite measurement in mm after 12-month treatment with JFO
INITIALS | GENDER | AGE T0 | OVERBITE T0 | OVERBITE T1 |
A. L. S. | F | 18 | (–1) | (–6,5) |
D. S. S. | M | 16 | (–2) | (3) |
A. D. A. | F | 34 | (–5) | (–4,5) |
W. H. O. | M | 14 | (0) | (2,5) |
J. P. A. | M | 15 | (–0,5) | (2) |
L. S. F. | M | 13 | (0) | (2) |
M. V. A. | M | 13 | (–4) | (2) |
M. B. M. | M | 15 | (–2) | (1) |
C. R. O. | M | 10 | (–7,0) | (–1,5) |
I. M. G. | F | 07 | (–7,5) | (–1,5) |
C. J. J. | M | 14 | (–4) | (1) |
M. A. F. S. | F | 07 | (–10) | (–5,0) |
I. A. S. | F | 12 | (–2,5) | (2) |
J. M. M. | F | 16 | (–3) | (3) |
A. S. F. | F | 14 | (–2) | (–1,5) |
S. P. J. S. | F | 26 | (–0,5) | (1) |
J. M. S. S. | F | 19 | (–3) | (1,5) |
3. Results
Table 1 presents sample description regarding gender and age and overbite measurements in millimeters in T0 and T1. Table 2 presents the values of the mean and standard deviation in T0 and T1 of the patients’ overbite and the P value resulted from mean comparison between T0 and T1.
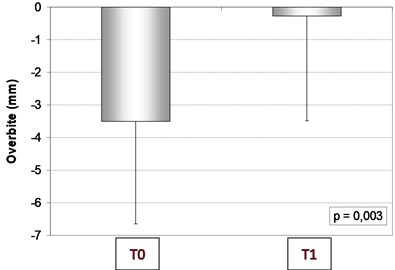
As shown in Table 2 and Graph 1 there was a statistically significant difference between overbite measurements in millimeters (P= 0,003), T1 values were higher than T0 values showing that JFO using Simões technic (SNs) was shown to be efficient to treat open bite in the sample studied.
Table 2Statistical comparison between initial (T0) and T1 results for overbite
T0 | T1 | Difference (T1 – T0) | p | |
Overbite (mm) | -3.50 ± 3.142 | -0.27 ± 3.219 | –3.23 ± 3.133 | 0.003 |
Data in mean ± standard deviation | ||||
Fig. 2Mean and standard deviation of overbite measures in mm at T0 and T1
4. Discussion
Up to now there is no report of self-correction of AOB in mixed or permanent dentition. In the deciduous dentition, depending on a range of factors, it sometimes self corrects, but there was no control group in the study and the results obtained have to be carefully analyzed.
Paoloni et al [4] reported that rapid maxillary expansion appliances combined with posterior bite blocks were shown to be efficient in the treatment of AOB in mixed dentition, and so were functional orthopedic appliances, therefore providing more tools for early AOB treatment.
In their paper, Santos et al [10] did not separate mechanical orthopedics and functional orthopedics. In the Fränkel technique. a functional orthopedic appliance (FOA) is used, the other types (crib, chin cup, and bonded spurs) are mechanical orthopedics appliances. Even with the Fränkel regulators there were results in the 95 % confidence interval of overbite improvement, a similar interval found in the present sample. A timely reminder is that they searched for RCTs, and the present investigation was a retrospective study, therefore their conclusion that high quality RCTs are needed is correct since they are really needed.
Surgical protocols are efficient to treat AOB in adults [8, 13], so are FOAs, the advantage of orthognathic surgery is that the height of the profile cannot be decreased by means of any other protocol. Du et al [13] used a CAD/CAM guide to position the mandible and maxilla during the surgery. As far as occlusion is concerned. both protocols are valid, whereas relative to profile height in adults, the surgical protocol is more efficient. Further investigations in growing individuals are necessary to verify whether the facial vertical growth can be controlled with the use of FOA.
The management of AOB with aligners has been scientifically proved [9, 14, 15]. According to Khosravi et al [14] the improvement in overbite is due to dental movement in the incisor region. Since FOA is also an efficient treatment and does not demand any overload on the region of the incisors in the treatment of AOB, this makes it an interesting option for treatment of individuals with periodontal loss of insertion in the incisor region. Moshiri et al [9] reported change of teeth for cephalometric landmarks and also reported the closure of the anterior nasal spine to the menton but did not explain whether this was due to mandibular or maxillary changes. In this investigation skeletal behavior of the face was not studied, only the improvement in overbite was studied.
Sambataro et al [3] reported the improvement in overbite with cervical headgear and control of vertical facial growth with this protocol. FOA is not only a more esthetic appliance but is also efficient for improving overbite in AOB treatment, however, there is no data regarding control of vertical facial growth in early treatment with JFO.
Using mini-implants for improvement of overbite has been reported [5, 16]. Both articles inferred results for molar intrusion. and reported mandibular rotation due to the molar intrusion. There are no data about posterior occlusal plane behavior in JFO and, as previously mentioned, no data about skeletal changes either.
5. Conclusions
The Functional orthopedic appliance was shown to be an effective tool to treat anterior open bite in the sample studied
Further studies, mainly Randomized Clinical Trials, with larger samples are necessary to confirm this result and to study stability and skeletal behavior in anterior open bite treated with jaw functional orthopedics.
References
-
C. Rijpstra and J. A. Lisson, “Etiology of anterior open bite: a review,” Journal of Orofacial Orthopedics / Fortschritte der Kieferorthopädie, Vol. 77, No. 4, pp. 281–286, Jul. 2016, https://doi.org/10.1007/s00056-016-0029-1
-
L. S. Todoki et al., “The national dental practice-based research network adult anterior open bite study: treatment success,” American Journal of Orthodontics and Dentofacial Orthopedics, Vol. 158, No. 6, pp. e137–e150, Dec. 2020, https://doi.org/10.1016/j.ajodo.2020.07.033
-
S. Sambataro et al., “Cephalometric changes in growing patients with increased vertical dimension treated with cervical headgear,” Journal of Orofacial Orthopedics / Fortschritte der Kieferorthopädie, Vol. 78, No. 4, pp. 312–320, Jul. 2017, https://doi.org/10.1007/s00056-017-0087-z
-
V. Paoloni, D. Fusaroli, L. Marino, M. Mucedero, and P. Cozza, “Palatal vault morphometric analysis of the effects of two early orthodontic treatments in anterior open bite growing subjects: a controlled clinical study,” BMC Oral Health, Vol. 21, No. 1, pp. 1–9, Dec. 2021, https://doi.org/10.1186/s12903-021-01886-5
-
H. E. Kassem and E. S. Marzouk, “Prediction of changes due to mandibular autorotation following miniplate-anchored intrusion of maxillary posterior teeth in open bite cases,” Progress in Orthodontics, Vol. 19, No. 1, pp. 1–7, Dec. 2018, https://doi.org/10.1186/s40510-018-0213-5
-
G. Janson, M. Rizzo, V. Laranjeira, D. G. Garib, and F. P. Valarelli, “Posterior teeth angulation in non-extraction and extraction treatment of anterior open-bite patients,” Progress in Orthodontics, Vol. 18, No. 1, pp. 1–7, Dec. 2017, https://doi.org/10.1186/s40510-017-0167-z
-
A. Vela-Hernández, R. López-García, V. García-Sanz, V. Paredes-Gallardo, and F. Lasagabaster-Latorre, “Nonsurgical treatment of skeletal anterior open bite in adult patients: Posterior build-ups,” The Angle Orthodontist, Vol. 87, No. 1, pp. 33–40, Jan. 2017, https://doi.org/10.2319/030316-188.1
-
M. Wang, B. Zhang, L. Li, M. Zhai, Z. Wang, and F. Wei, “Vertical stability of different orthognathic treatments for correcting skeletal anterior open bite: a systematic review and meta-analysis,” European Journal of Orthodontics, Vol. 44, No. 1, pp. 1–10, Jan. 2022, https://doi.org/10.1093/ejo/cjab011
-
S. Moshiri, E. A. Araújo, J. F. Mccray, G. Thiesen, and K. B. Kim, “Cephalometric evaluation of adult anterior open bite non-extraction treatment with Invisalign,” Dental Press Journal of Orthodontics, Vol. 22, No. 5, pp. 30–38, Oct. 2017, https://doi.org/10.1590/2177-6709.22.5.030-038.oar
-
E. Marcílio Santos et al., “Functional orthopedic treatment for anterior open bite in children. A systematic review of randomized clinical trials,” Journal of Orofacial Orthopedics / Fortschritte der Kieferorthopädie, pp. 1–10, Apr. 2022, https://doi.org/10.1007/s00056-022-00388-5
-
W. A. Simões, Ortopedia Funzionale dei Mascellari. (in Italian), Orbetello, 2010.
-
O. Santiago Jr and I. P. M. Santiago, Atlas de Construção de Aparelhos Ortopédicos Funcionais. (in Portuguese), Ribeirão Preto.
-
W. Du, G. Chen, D. Bai, C. Xue, W. Fei, and E. Luo, “Treatment of skeletal open bite using a navigation system: CAD/CAM osteotomy and drilling guides combined with pre-bent titanium plates,” International Journal of Oral and Maxillofacial Surgery, Vol. 48, No. 4, pp. 502–510, Apr. 2019, https://doi.org/10.1016/j.ijom.2018.08.012
-
R. Khosravi et al., “Management of overbite with the Invisalign appliance,” American Journal of Orthodontics and Dentofacial Orthopedics, Vol. 151, No. 4, pp. 691–699.e2, Apr. 2017, https://doi.org/10.1016/j.ajodo.2016.09.022
-
K. Harris et al., “Evaluation of open bite closure using clear aligners: a retrospective study,” Progress in Orthodontics, Vol. 21, No. 1, pp. 1–9, Dec. 2020, https://doi.org/10.1186/s40510-020-00325-5
-
A. Cambiano, G. Janson, D. Lorenzoni, D. Garib, and D. Dávalos, “Nonsurgical treatment and stability of an adult with a severe anterior open-bite malocclusion,” Journal of Orthodontic Science, Vol. 7, No. 1, 2018, https://doi.org/10.4103/jos.jos_69_17

