Abstract
Micro-rhinic Dysplasia is a common finding in patients who seek for dentofacial correction have several degrees of facial growth commitment and can be associated with another growth syndromes like the Rotation Syndrome, for instance, which may increase the degree of difficulty in corrective treatment of malocclusion. The most challenging malocclusion treatment in an individual with Micro-rhinic Dysplasia is the anterior open bite, mostly when associated with prognathism. The aim of this manuscript is to show through patients records the clinical and cephalometric characteristics of Micro-rhinic Dysplasia alone or associated with other craniofacial growth alterations and their consequences in malocclusion treatment.
In the context of our discourse about the inter-maxillary bone problems, I want to introduce to you a triad of symptoms which we called for a while “Micro-rhinic Dysplasia” [1].
The aspect of the affected patients is highly characteristic and well known to all experienced practitioners. Today’s remarks shall define this syndrome with the aid of extreme cases and clarify the classical triad of the cephalometric symptoms, the so-called Rotational Syndrome [1].
I consider it to be the more important as this syndrome is not restricted to a few dysplastic cases of mostly scientific interest but is relatively common. In about 30 % of my clinical cases, it can be found in a more or less pronounced degree.
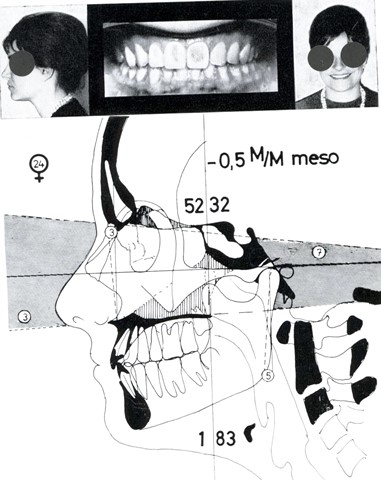
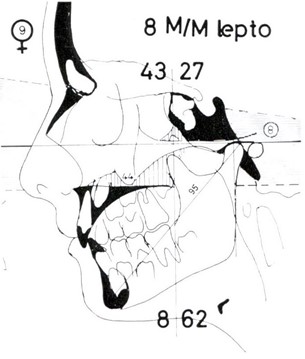
Fig. 1The main external symptoms are the short nose where the nostrils are visible from the front, and the short upper lip
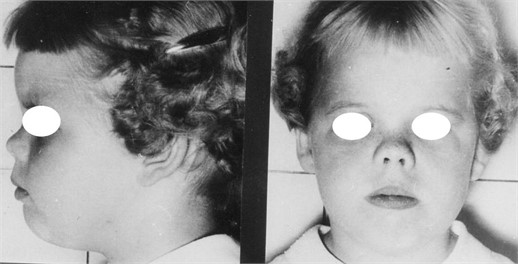
Hence it has a basic importance for the understanding of the morphological conditions of certain maxillary anomalies and for the therapeutic intervention. The symptoms accessible at external examination are the following (Fig. 1):
1) A small nose with an upward directed base with the nostrils visible at a natural head position.
2) A low, in some cases even “dished-in” mid face.
3) Often an open mouth with a seemingly or really short upper lip.
4) Sometimes an anti-mongoloid slant of the eyes,
5) Often protruding or sometimes even crippled ears.
The intra-oral examination reveals regularly symptoms which affect in a more or less pronounced way the inter-maxillary bone but can vary considerably in their manifestation pattern. The most common and easiest to understand is the hypoplastic Frontal Open Bite. However, the Inter-maxillary Hypoplasia can express itself also in a narrow, crowded front with or without ectopic canines. In certain cases, we can observe a frontal crowding with a deep bite or even a Class III [2].
The cephalometric symptoms of the Micro-rhinic Dysplasia can be listed as follows [1]:
1) a forward-upward tilted nasal plane.
2) a forward-upward hyperflected mandible.
3) an increased inclination of the anterior part of the cranial base as presented by the N-S line.
4) as additional cephalometric finding, we see sometimes a diminished or missing pneumatisation of some sinuses.
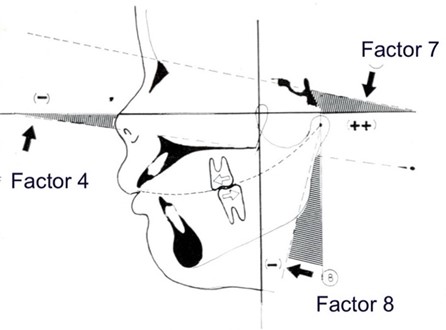
To simplify the communication, I will call for the rest of this text the inclination of the nasal plane “Factor 4”, the flexion of the mandible “Factor 8” and the inclination of the N-S line toward the Frankfurt Horizontal “Factor 7” (Fig. 2) [1].
Considering the tracings of our dysplastic cases with the Factors 4, 7, and 8, they all seem to be rotated in relation to the FH reference system, therefore we also refer to the Micro-rhinic Dysplasia as the “Rotational Syndrome”.
Here is seems useful to add some general remarks about the recurrent question if the FH or the NS line are preferable as a reference system. First of all, we have to consider that the FH line represents lateral parts of the visceral skull, namely the zygomatic arch and the petrous bone which again are essential for the position of the mandibular joint. On the other hand, the NS line represents medial sections like the ethmoid bone, the sphenoid bone, and further the vomer and the maxilla.
As the Micro-rhinic Dysplasia obviously follows a set pattern of shifting the medial parts of the visceral skeleton against the lateral parts, we will have to consider both lines.
Fig. 2The rotational syndrome of the micro-Rhinic Dysplasia (“Cephalometric Triad”, Bimler). 1. Upward-tilted ANS-PNS line (Factor 4); 2. Hyperflected Mandible (Factor 8); 3. Increased inclination of the NS-line (Factor 7). The shift of the dental skeleton units against each other causes a Class II occlusion
It is undisputed that reference points like N or S on lateral head plates can be identified and reproduced with greater precision by different researches; however, this does not mean at all that the NS line is therefore especially appropriate as a base line for a system with which we want to study with benefit and profit the deviations of the structure of the visceral skeleton. We do not believe so. The informational value of a tracing based on the FH line is by far superior, as also the studies for this research have been showing.
I believe that my venerated teacher A. M. Schwarz was the first to draw the attention to such rotational phenomena and called the findings “dentition slew”. He tried to explain the situation that we should imagine the dentition separated from the visceral cranium along the palatal plane, and shifted in toto around a suspension point at the anterior cranial base.
This might be acceptable for a mere introductory didactical purpose but cannot be kept up with further investigation. Soon it becomes obvious that maxilla and mandible act quite independently. Concerning the dentition, this becomes very obvious by the sagittal shift of the upper and lower dental arches along the Curve of Spee, by which we can understand the occurrence of a Class II [2].
While the dentition can well be considered a functional unit but not an anatomical one, it is no surprise that its skeletal units act independently. Therefore, it proved necessary and useful to check the behaviour of maxilla and mandible, of the anterior cranial base and the joint region independently from each other. We represent them by the Factors 4, 7, and 8, and the linear measurements of the maxillary length, the mandibular length and the T-TM distance. Under these aspects we want to consider now some sample cases. Our first case shows the already familiar 8-year-old girl from the first picture. I selected her because she shows in an extreme way the main feature of this complex, the small and upward directed nose which gave the name to the syndrome (Fig. 3).
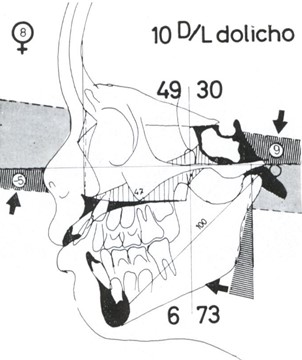
Fig. 3Micro-rhinic Dysplasia – Orthognathic Mid Face. The Formula “10 D/L dolicho” shows the typical D/L shift which are predominant in Frontal Open Bite cases. Our Factor Analysis with the negative F4 and F8 reveals the mechanism of the facial dysplasia as a clockwise rotation, in relation to FH
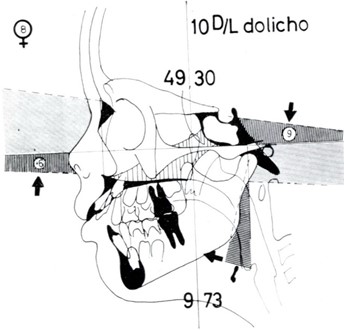
The Factor 4 representing the disturbed mid face shows a high negative value of – 6°. Additionally, the pre-maxillary bone is distinctly tilted upwards and, by a kink, distinct of the maxillary part of the nasal plane. It is easy to understand that also the upper incisors will be protruded together with their tilted base, and the problem of the Class II at the posterior teeth appears in a new light now.
Of course, they will also be shifted in an anterior position together with the front teeth, and we see that, notwithstanding a prolonged closing movement, the dentition can only get in occlusal contact in a Class II position as the mandible cannot catch up with the “rotation” of the maxilla. Within the “dentition slew concept” it means a shift of the dental arches in a sagittal direction along the Curve of Spee (Fig. 2). But then we must never lose sight of the fact that this description of a slew against an imaginary normality only has a hypothetical character and never could be substantiated in a longitudinal study of any individual patient.
Like in most cases, the frontal cranial base is involved and the value for the factor 7 of 9° is slightly higher than the average value which in harmonious faces is 7°. In this patient we find in all three Factors 4, 7, and 8, a change in the same direction which we describe as a clockwise rotation towards the Frankfurt Horizontal.
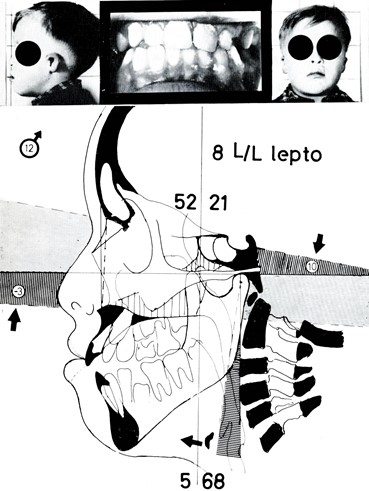
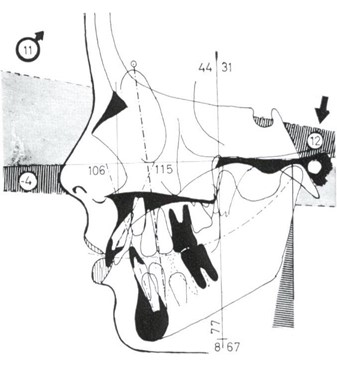
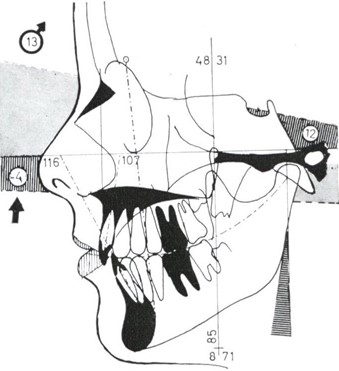
Our next case, a nine-year old girl (Fig. 4) shows a considerable increase of the intermaxillary or maxillary hypoplasia at the intra-oral examination, and externally the slanting eyes are noticeable.
Fig. 4Micro-rhinic Dyplasia – Rotational Prognathia. The formula “19 M/L lepto” shows the higher convexity of the face. The Factor Analysis reveals this partly as a prognatic maxilla (positive F1: N-A), partly as a posterior position of the chin (high F2: A-B). The extreme inclination of the cranial base F7 (N-S) towards the FH indicates that it is involved in the rotational process. This is expressed also by a steeper Clivus Inclination (F8: tangent to posterior board of the Clivus). This increases the angle between Clivus and Maxilla and puts it into the meso-prosopic values (“M” of the formula). A high maxillary alveolar process stops the compensatory closing movement of the mandible, hence the F decreases and the F2 increases, so does the Open Bite. The consequence is a vertically high face (“lepto”). The T-TM distance of 29 mm belongs to the medium size range
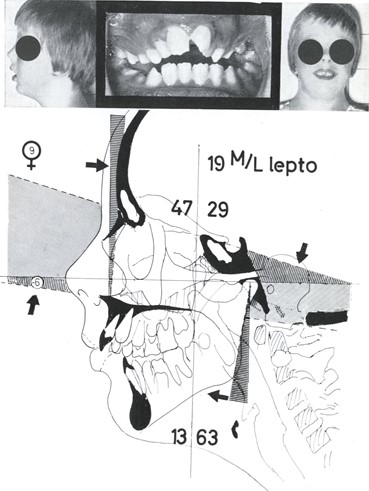
Analysing the cephalometric tracing, the Factor 4 – maxillary rotation – shows the same value like the previous case, i.e. – 6°, however here the cranial base is much more involved in the rotational process: the NS line shows an inclination of 16° towards the FH which belongs unquestionably to the highest values at all.
In this case, the rotational phenomenon has the additional effect of the development of a true prognathism in the anthropological sense, with A-point ahead of N-point. We call these cases of distal bite also “rotational prognathism”. Checking Factor 8 – the flexion of the mandible – we see also here a pronounced hyperflexion, but to a lesser degree that in the previous case. The reason for this is obvious for the expert: a relatively high alveolar process in the molar region, which is very typical for such Structural Open Bites, and by which the closing movement of the mandible is stopped earlier.
From a functional viewpoint, it is interesting to observe over and over again how the molars that bear the entire masticatory pressure do not yield at all to this functional pressure. A lowering of the bite by grinding the clinical crowns will be compensated soon by growth.
The only way to improve such an open bite due to a rotational prognathism, in our experience using Bimler appliances [3], is the extraction of the first molars. By this the Curve of Spee is deepened, the only mechanism to compensate the skeletal deviation which is the underlying cause of the Open Bite.
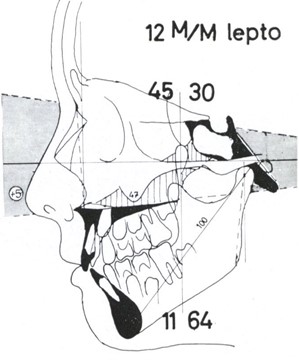
Our next case (Fig. 5) is a progenia in an 11-year old boy, who displays again the typical facial features of the slanted eyes, the protruding ears, small nose and open mouth. Looking at him, the progenic dentition is not even very obvious.
Fig. 5Progenic Class III. Our 11-years old patient shows the typical face with the small nose, open mouth, slanted eyes and even the protruding ears. The frontal cross bite is hardly visible. We find again our cephalometric triad of: negative F4 = –4°, increased F7 = 12°, negative F8 = –11°. The TTM distance of 24 mm is very short
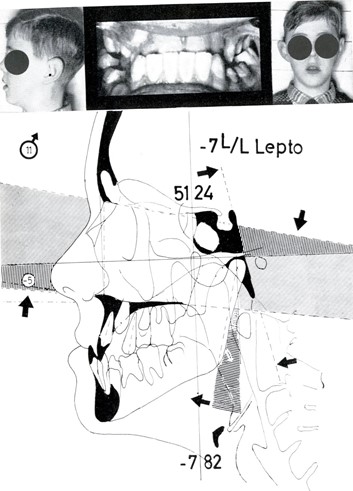
In the x-ray evaluation, we find again our 3 components:
1) a negative Factor 4.
2) a high Factor 7 of 12°.
3) a negative Factor 8.
The last one shows that also here, the mandible is hyperflected to compensate the anterior height deficit in the midface. When the patient does not close his teeth but leaves the mandible in the physiological rest position, the posterior margin of the mandible is situated more or less vertical to FH.
It might be interesting to know that just such progenic cases were the first to draw our attention to the different degree of flexion of the mandible, as they show a particularly high difference between the physiologic rest position and the occlusion.
A further morphologic characteristic, which contributes to the manifestation of a progenia and regularly can be found in Class III cases, is the pronounced shortening of the T-TM distance. The distance between the posterior margin of the maxilla and the joint, also here, is reduced to 24 mm using the standard measurements.
The stereotype occurrence of similar symptoms in the structure of the visceral skull now leads to the question if we could not find a similar origin for these similar changes. Especially the exterior appearance with the small saddle nose suggests to look for some growth inhibition. Accordingly, we controlled a number of deformities where the origin is already more or less established. First example is a Chondro-Dystrophy, the well-known disorder where the growth of the long bones is considerably reduced by a disturbance of the cartilage growth (Fig. 6).
For the visceral skull, Chondro-Dysplastic dwarfs are characterized by tower skulls (Oxycephaly) and saddle noses. With our analysis we see the usual picture with the negative Factors 4 and 8, while here we do not find the characteristic flattening of the cranial base, whereas we see a reduction of the T-TM distance to 25 mm.
Next, I want to present a case of Dysostosis Cranio-Facialis (Pseudo-Crouzon), a boy with an operated cleft lip and above all heavily crippled ears (Fig. 7). With a fully develop intelligence he suffered at about 20 years of age an increasing hearing loss, while on the x-ray picture the Porus Acusticus was not visible any more, the roentgenologic sign for an increasing narrowing of the external acoustic meatus which was also clinically established.
Fig. 6Chondro-dystrophic dwarf. The stereotype appearance of the same syndromes suggests a growth inhibition as we see it also in this case of dwarfism. Indeed, we find the negative F4 and F8, the small saddle nose and a short TTM

Fig. 7Dysostosis Cranio-Facialis (Pseudo-Crouzon). This 12-year old boy had additionally a cleft lip. He shows the classic triad and also a very short TTM distance
Analyzing the facial structure, we find the typical triad in full, a negative Factor 4, an increased Factor 7, and a negative Factor 8. The T-TM distance is reduced to 21 mm and leads our attention to the area where the predominant changes can be found, namely towards the shortened Clivus as indication of a growth inhabitation in the region of the sphenoid and the occipital bones. This is also the reason for the very extraordinary tilt of the foramen magnum, among other features.
The localisation makes us think immediately of a disturbance in the area of the rhombencephalic induction apparatus, the so-called occipital organizer which today is believed to be responsible for an entire group of oto-cephalic development disorders.
Though the causes for the two disturbances are obviously different, the cephalometrically ascertainable symptoms at the visceral skull show a stereotype uniformity.
The last two cases were clearly inhibition deformities, though from different origin. The following case is a ten-year old girl of American nationality with a mix of Levantine, Native American and African blood (Fig. 8). Neither external nor intra-oral examinations show a sign of a growth inhibition of any kind, but here are just the skeletal parts of non-matching forms and shapes combined in one individual.
Fig. 8Mixed race child. Phenocopy of the Pseudo-Crouzon case in an otherwise normally developed child with a very dissimilar racial background of African, Indian and European family background
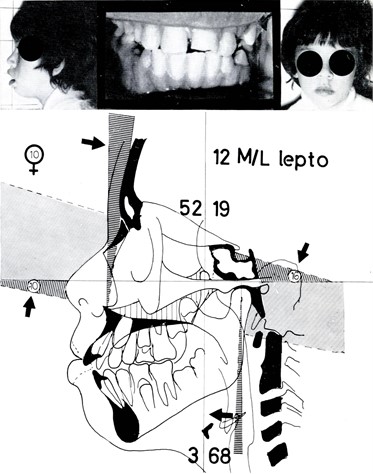
The striking observation in the sequence of the last two cases is how the cephalometric picture of the development inhibition phenotype is repeated in the little girl. From our triad, the negative Factor 4 of – 10° and the steep cranial base of 16° are especially noticeable, while Factor 8 is more or less unaffected. The importance of the reduced T-TM distance is very conspicuous here, as the very short value of only 19 mm helped in this case to achieve a Class I molar relation, in spite of the strong anthropologic prognathism with a simultaneous orthodontic rotational prognathism. In this respect, our case is a classic example how the clinical picture at which the dentist is looking can be caused by a variety of structural components which can either – in our favourable case – compensate each other or vice versa can lead to extreme deviations.
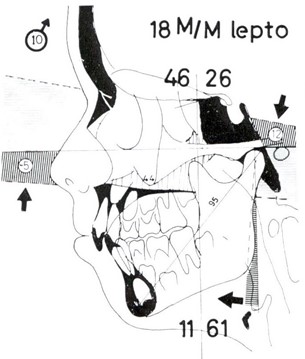
Now I slowly want to lead you away from pathological extreme cases to the every day cases of the daily practice, und may present to you a 16-year old boy (Fig. 9). He shows, beside the now well-known external feature of a small saddle nose, only the Factor 4, the nasal plane, rotated upwards in the usual manner, while the other Factors behave in an almost normal way. The skeletal deviation manifests itself clinically in a very treatment-resistant open bite. Of course, at a local observation, immediately a tongue interposition was visible and originally taken as the cause for the open bite. Meanwhile we got doubts to overvalue functional causes at the presence of distinct cephalometric findings.
Our next example (Fig. 10) shows a harmoniously built visceral skull with a respective facial type. Here you see, as to be expected in undisturbed cases, the Factor 4 running either parallel to FH or slightly downward inclined as in this example. The NS-line inclination shows the classic “norm” value of 7° and Factor 8 stay under 5°, thus giving the impression that the posterior margin of the maxilla hangs perpendicularly to FH.
Fig. 9Every day patient. Leaving the pathologic extremes aside, this 16 yrs. old boy is an average patient. His persistent open bite can be related to his skeletal structure
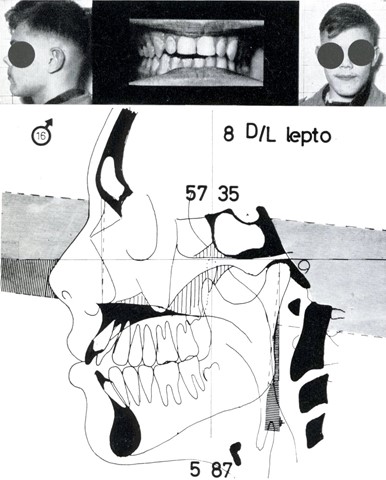
Fig. 10Normoplasia. As a comparison, here a harmoniously built visceral skull of the mesoprosopic type with a correct occlusion
I put in this example of a normal case to give you a chance to compare it with our initial case. We take this case now to clarify the consequences of the Rotational Syndrome by erasing it on the tracing: we correct it in a speculative way to a normo-plastic condition and put both side by side for comparison (Fig. 11).
We used in the “corrected” tracing the same outline and sizes like in the original. After tracing the skeletal base and the joint region, we put the mandible in a position like in normal cases, this is with an almost perpendicularly hanging posterior margin. Then we compensated the upward rotation of the maxilla the other way round, and automatically the protruded incisors and the Class II molar relation disappeared. Of course, the mid-face now showed a big deficiency in height which we had to fill by inserting a middle size nose. The result of this reconstruction is a harmonious dentition in a harmonious face. Besides we can see how the changed inclinations of single bones change their projected standard measurements in one way or the other.
Fig. 11Micro-rhinic Dysplasia – Meso-rhinic Normoplasia. Comparison of the Fig. 1 and 3 and a hypothetical tracing of the same case with her anatomical units in a normoplastic layout with a meso-rhinic nose. Thus, the Cl.II and the open bite disappear automatically
a) Micro-rhinic Dysplasia
b) Meso-rhinic Normoplasia
Fig. 12Micro-rhinic Dysplasia – Meso-rhinic Normoplasia. Comparison of two siblings with same-size anatomical units in a dysplastic layout in the brother and a normoplastic arrangement in the sister, as a confirmation of the previous hypothetical tracing, via respective findings in the clinical cases
a) Micro-rhinic Dysplasia
b) Meso-rhinic Normoplasia
Of course, now you have every right to ask if such a speculative reconstruction is permitted and what sense it would have. So, I selected from my collection of cases a pair of siblings. The older brother shows all signs of a Micro-rhinic Dysplasia, while the sister, one year younger, had a normoplastic development with about the same size for the anatomic units (Fig. 12).
You can see with this example the equivalence of my speculative reconstruction, now as real changes in the development of otherwise very similar family members. As opposed to the negative Factor 4 of –5° in the brother, the sister has a value of 0°. Compared to the augmented Factor 7 of 12° in the dysplastic boy, the sister shows an almost normal value of 8°; the Factor 8 which is clearly increased in the brother, is normal in the sister.
In the dentition, the micro-rhinic dysplastic case presents a Class II molar relation, while the normoplastic case has a Class I occlusion.
With this presentation I want above all underline that the distal bite may not be understood unilaterally as an abnormal position of the mandible, and that the skeletal conditions leading to a Class II molar relation can indeed be manifold.
Unfortunately, here I cannot go into details of the clinical possibilities to compensate a Micro-rhinic Dysplasia, especially under which circumstances we can count with a positive or a negative influence to our prognosis. Future papers will report about that.
Finally, I want to present you only one case of Micro-rhinic Dysplasia deep bite where we find all symptoms of our triad fully formed. We call this a “paradox deep bite” because here the clinical symptoms of a Class II deep bite are combined with a skeletal structure in the visceral skull as we usually find them in open bite cases (Fig. 13 to 15).
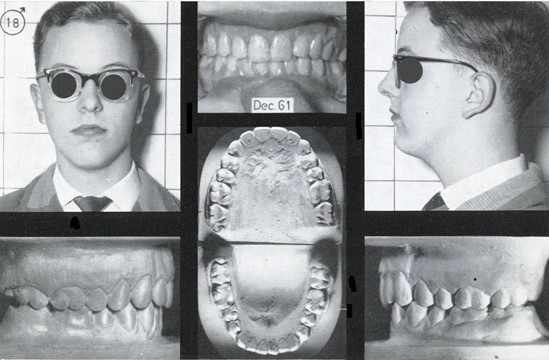
Fig. 13Micro-rhinic Deep Bite in Class II. Start of treatment and the dento-alveolar compensation after two years. The dysplastic skeletal structure did no change
a) Micro-rhinic Deep Bite
b) Dento-alveolar compensation
The follow-up x-ray after two years shows that the dysplastic structure, the Factors 4, 7, and 8, had not changed. Nevertheless, we achieved a correct occlusion in the classic sense by up righting the upper incisors distally and proclining the lower incisors. Probably the hidden open-bite-structure as expressed by the negative Factor 4 has helped to raise the bite. Formerly we would have credited this to one or the other treatment method applied.
Summarizing we should say that we tried with this presentation of the Micro-rhinic Dysplasia to define a stereotype reaction within the visceral skull by a triad of symptoms, and to underline the connection of the clearly visible external features with this so-called Rotational Syndrome. Thus, the clinical practitioner should be enabled, once faced with the external symptoms, to check for the respective skeletal deviations and keep them in mind for his treatment plan and prognosis.
Fig. 14Previous patient, 11 yrs
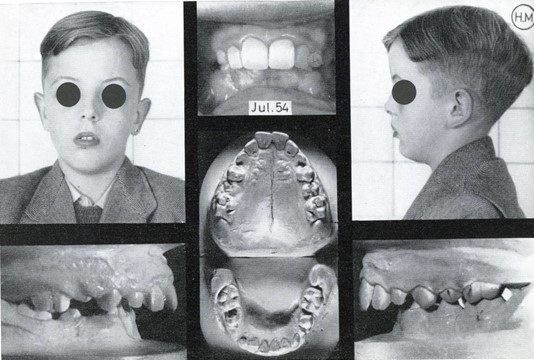
Fig. 15Patient at 18 yrs. long term control
References
-
H. P. Bimler, “Die bedeutung des fernröntgenbildes,” Fortschritte der Kieferorthopädie, Vol. 20, No. 3, pp. 256–273, Sep. 1959, https://doi.org/10.1007/bf02286320
-
H. P. Bimler, “Some thoughts about orthodontics and TMJ troubles,” The Functional Orthodontist, Vol. 17, No. 4, pp. 21–24, 2000.
-
H. P. Bimler, “The Bimler Appliance,” in Removable Orthodontic Appliances, London, 1977.
About this article
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.

