Abstract
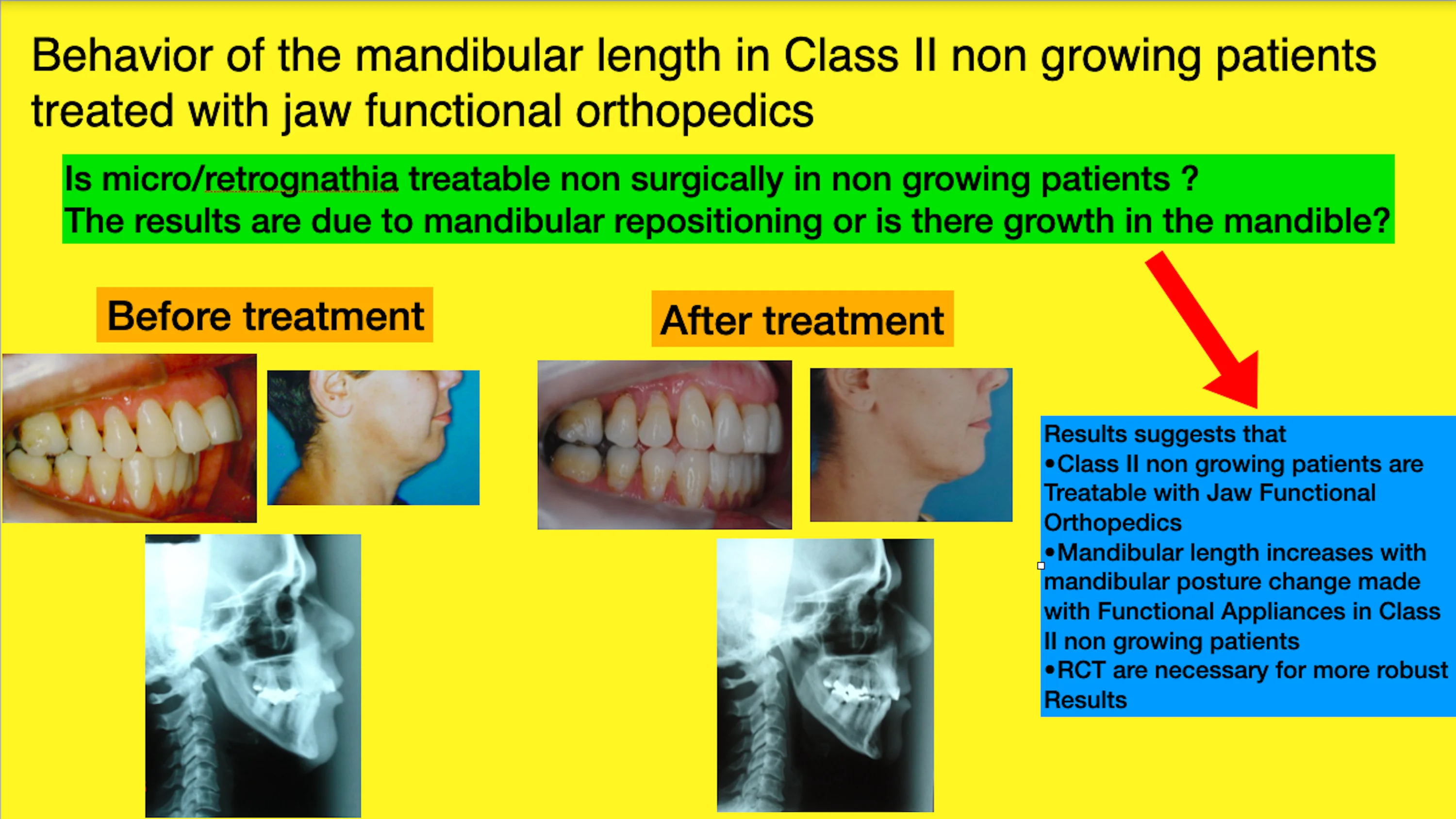
Class II treatment is the leader of seeking for dentofacial correction in offices all around the world due, mainly, to facial esthetics impairment caused by this malocclusion. Mandibular forward repositioned is needed for the majority of this treatment. Jaw Functional Orthopedics (JFO) is a recognized protocol to treat Class II in growing patients. The aim of this investigation is to study the behavior of mandibular length in class II non-growing patients treated with JFO. Distance between Gonion and Mento were measured in lateral teleradiographs at T0 and T1 (from 18 to 21 months of treatment) of non-growing class II patients under treatment with JFO and mandibular supplementary growth was found (P = 0,006). In the sample studied jaw functional orthopedics showed to be efficient to correct the overjet in class II non-growing patients. Mandibular advancement with functional orthopedic appliances promotes a supplementary mandibular growth in non-growing patients. Further studies are necessary for a better comprehension of the subject.
Highlights
- Mandibular growth in non growing patients with jaw functional orthopedics
- Mandibular growth in non growing patients with mandibular advancement appliance
- Retrognathia treatment in non growing patients
- Class II treatment with mandibular retrognathia in non growing patients
1. Introduction
Since Angle’s time, no subject has had as much repercussion in the literature and clinical practice as Class II treatment, because, although not the most frequent malocclusion in the population, it represents the majority of patients seeking treatment [1]. In class II malocclusion the maxilla is more frequently in neutral or retruded position, and only a small percentage of cases present skeletal maxillary protrusion. On the other hand, skeletal mandibular retrusion is the characteristic most commonly found in these patients [2]. For such, mandibular advancement is the treatment protocol indicated for the majority of Class II patients.
The significant commitment of facial aesthetic is the main reason why class II is the malocclusion most leads to the search for corrective treatment [1]. Although the perception of beauty is highly subjective it is a common sense that retrognathia impacts significantly facial aesthetics [3-5]. One of many benefits of mandibular advancement is the improvement of facial esthetics [4, 5].
Besides esthetic commitment there are some another significant problem that class II malocclusion brings to the individual. Almasan et al. [6] reported a relationship between class II malocclusion, temporomandibular disorders and cervical posture in studies that show MRI bone and soft tissues change, although literature still shows contradictory opinions. Sandoval et al. [7] described the relation between retrognathia and cervical lordosis and Zokaite et al. [8] reported an increase of cervical inclination and head upright position. Watanabe et al. [9] reported the relationship of the height of the atlas dorsal arch of cervical vertebrae with anteroposterior position of the mandible. In children, Klostermann et al. [10] reported changes in the pelvic region with mandibular advancement promoted by Frankel type II appliance.
About Class II treatment Planas [11] stated that one cannot believe in genetic predetermination in mandibular growth, nor in mandibular development discrepancies neither in invariability of mandibular basal bone. Moss reported that bone tissue does not receive direct genetic information in its growth and development process, but They are received from the surrounding environmental, and that central nervous system and the musculature acts more in the facial skeleton than the inherited. As early as 1902, Robin reported improvement of overjet advancing the mandible with his activator. Austro-Martinez et al. [13] reported not only Class II malocclusion correction but also stability of mandibular advancement one year after treatment.
Adult treatment is one of the most challenging and studied subject nowadays. Alikhani et al [14] reported that adults respond to orthodontic treatment but have a significantly slower rate of tooth movement than adolescents, for such, there are some papers prescribing mechanical vibration to accelerate tooth movement in adults [15-17].
Espinosa et al. [18] reported that in non-growing patients a normalization of class II malocclusion mainly through dentoalveolar changes, only with use of Herbst appliance some minor forward change of the mandible was noted. DiBiase et al [19] reported, studying cephalograms, that there are differences in results according to the appliance used to mandibular propulsion in adolescents, individuals using Twin Block had more mandibular growth than using Dynamax during treatment and in the follow up period still there are some changes resulting in more growth in individual with Dynamax use than Twin Block. Mohammed et al. [20] in a systematic review also found difference in results of treatment with prefabricated myofunctional appliances and activators.
The aim of this investigation is study the behavior of the mandibular length in non-growing individuals with retrognathism treated with mandibular advancement with FOA.
2. Material and methods
A case series study was made searching in the data base of the Specialization Course in Jaw Functional Orthopedics of the Brazilian Dental Association ABO, Sub-Section/Muriaé-MG, in a universe of 257 patient treated, 45 (17.5 %) had class II with positive overbite. The age inclusion criteria used, was Martins et al [21] in their craniofacial growth atlas.
The inclusion criteria used was at least 16 years and 6 months old at the day when functional orthopedic appliance (FOA) was installed in mouth based on the group report by Martins et al. [21] were significant mandibular growth ceased, have mandibular retrognathia and correct use of the functional orthopedic appliance. Twenty individuals matched the inclusion criteria. Eleven individuals were discarded for non-provision of radiography for the collection of data on the right time interval. Nine individuals were studied ages ranging from 16 years and 6 months to 39 years and 1 month. There was no sample size calculus.
Compound Planas Indirect Tracks appliance were used to treat the individuals. The appliances were constructed in the laboratory according to the instructions of Simões [23].
Lateral cephalograms were traced to study the behavior of mandibular length during class II treatment of jaw functional orthopedics at T0 (radiographies before use of functional orthopedic appliance) and T1 (radiographies from 18 to 21 months of treatment). In order to match the sample with Martins’ growth atlas [21], mandibular length was studied measuring the distance Gonion (Go) – Menton (Me) and the parameters for marking the points were the same described in the atlas. Statistical analyzes of the data was made using the t-test for paired samples at a significance level of 5 %.
Clinical measurement of the overjet was made monthly with a pachymeter (Fig. 1). Overjet measurement at T0 (before installing the functional orthopedic appliance in the mouth) and T1 (day the individual brought the second lateral radiography) by the students properly calibrated can be seen in Table 1.
The measurements were obtained by the students, properly calibrated, without knowledge of the subsequent use of the data, monthly, having as reference for all, dental elements 21 and 31, as can be seen in the photos above. Comparing the measurements of the overjet, it was concluded that there was a decrease in overjets, ranging from 0.5 to 7mm.
Statistical analyzes of the data was made using the t-test for paired samples at a significance level of 5 %.
Fig. 1Clinical measurement of the overjet

3. Results
Data obtained can be seen in Table 1. The assumption of abnormality was verified through the Shapiro-Wilk test. As the initial and final Go-Me (mm) values presented approximately normal distribution (p> 0.05), in the comparison between the means at T0 and T1.
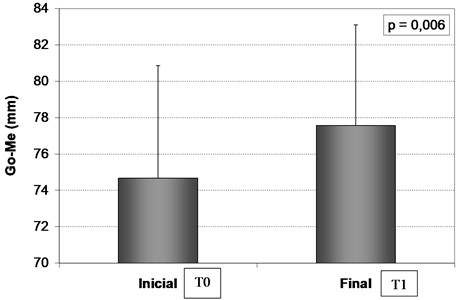
Table 2 and Fig. 2 show the values of T0, T1 and difference standard deviation for Go-Me (mm), the P-value resulting from the comparison between the means obtained through the t-test for paired samples is P = 0,006 showing statistical difference of mandibular length after 18 to 21 months of use of FOA.
Table 1Age at the FOA installation in mouth, Overjet measurements at T0 and T1 and Go-Me measurements at T0 and T1 in millimeters
Individual | Age | Overjet T0 mm | Overjet T1 mm | Go-Me T0 mm | Go-Me T1 mm |
1 | 16 y 6 m | 5,0 | 4,0 | 72 | 75 |
2 | 38y 5 m | 4,0 | 3,5 | 82 | 86 |
3 | 29y10m | 11,0 | 7,0 | 71 | 72 |
4 | 39y 1 m | 9,5 | 2,5 | 79 | 82 |
5 | 17 y 3 m | 4,5 | 3,0 | 73 | 74 |
6 | 16 y 10 m | 6,0 | 4,0 | 75 | 78 |
7 | 31 y 10 m | 9,5 | 6,0 | 85 | 85 |
8 | 38 y 4 m | 6,0 | 3,0 | 68 | 71 |
9 | 33 y 3 m | 10,0 | 6,5 | 67 | 75 |
Table 2Statistical comparison between Go-Me measurements at T0 and T1 in mm.
T0 | T1 | Difference (T1 – T0) | p | |
Go-Me (mm) | 74,67 ± 6,185 | 77,56 ± 5,548 | 2,89 ± 2,315 | 0,006* |
Data in ± standard deviation * Statistically significant difference | ||||
The results indicated that the Go-Me (mm) values after treatment were statistically higher than the initial values (p= 0.006). The mean difference between the final value and the initial value was 2.89 ± 2.315 mm, indicating that the patients had an increase in the Go-Me value (mm) over time while using FOA.
Fig. 2Mean and standard deviation of Go-Me measurement (mm) at T0 and T1.m
4. Discussion
The current investigation with its limitations (no sample calculus and no control group) suggests that there a mandibular length growth in retrognathic individuals treat with functional orthopedic appliance. Unfortunately, the results cannot be fully discussed with the literature because no other study with statistical analyzes of retrognathia treatment in non growing individuals treated with JFO was found on the literature. The discussion below will be made with investigations of growing retrognathic individuals treated with functional orthopedic appliances.
Regarding some aspects that justify Class II treatment such as increase attractiveness [4, 5] and consequently self-esteem, helping prevention or assist in the treatment of spinal column problems [6-8, 10], TMD treatment [26], they are not analyzed in the present study.
Mandibular growth due to JFO treatment of Class II with mandibular forward positioning in growing individuals is shown in the literature [4, 5, 13, 18-20, 22]. The type of appliance used in the class II treatment influences organism responses in its own way [22]. None of the papers recovered can be entirely compared with the present studies recovered investigated responses of Planas appliances, neither in non growing individuals as done in this investigation. Despite of that, results found in the literature consulted [4, 5, 13, 18-20, 22] are similar to those found on the current investigation.
The sample of this investigation has a wide age range and the control group used was Martins et al [21] atlas that reports the end of ontogenetic mandibular growth in Brazilians at the age of 17. Based on these results must be analyzed very carefully and, naturally Randomized Clinical Trials studies are necessary.
Another point to be observed with caution on class II treatment planning is what kind of mandibular posture change (MPC) [23] will be used and which appliance with tis respective modus operandi used on the treatment. This is a very important point to analyze on the methodology of the papers published about class II treatment with mandibular advancement. In non-growing patients class II treatment results differs from dentoalveolar compensations to orthopedic effect on the mandible depending on the type of appliance used [18].
According to Riddle et al. [24] Much has to be studied about the behavior of the mandible when subjected to biomechanical alterations. Gender and facial biotype influence the mechanical behavior of the mandibular ramus length. Clinically, it was shown that different FOAs stimulate different responses in the organism. Of course, treatment stimulation has to be lighter and treatment tends to take a longer time in non growing individuals this is based on personal clinical observation and scientifically reported [14].
About adult treatment it seems, based that age does not affect the kind of response, FOAs stimulate in the mandible, probably the number of cells involved in the process may be affect and the time of treatment is extended, but further investigations are required to verify these statements [24] what is in accordance with the findings of this investigation where elongation of mandible was detected during mandibular advancement with FOA in non growing individuals. Beherents [25] showed modifications on the craniofacial skeleton in aging people with any additional intervention (use of any dentofacial corrective protocol), showing biological activity in the bones. This fact may explain the capacity of the mandibular bone response when submitted to mandibular advancement with FOA, but changes are relatively small and takes about 40 to 50 years. The mandibular growth obtained in the sample studied does not seem to be result of this craniofacial remodeling, it seems to be due to the use of JFO in class II treatment.
Regarding stability of treatment there is a crucial point that is time. According to Simões [23] the mandible should be kept in the desired position twice the time it took to memorize in the neuromuscular system this position. For instance, if the mandible reaches the correct orthopedic position in 8 months it should be kept for 16 months more to complete osseous remodeling and central nervous system works properly in the new mandibular position. Due to limitation of observation time between T0 and T1, treatment stability was not studied in this investigation, but Class II treatment with MPC (mandibular forward positioning) in brachyfacial growing stability was reported [13]. Investigation about stability of non-growing class II patients treated with mandibular advancement is necessary.
Biologically, the findings of the current study are justified by the studies of Petrovic et al. [27] which showed the correlation of mandibular anterior repositioning and retrodiscal pad activity raise and Rabie et al. [28] which reported that forward mandibular positioning was found to solicit a sequence of cellular events leading to increased vascularization and subsequently new bone formation resulting in enhanced condylar growth.
The data obtained in the sample studied suggests the JFO is efficient in class II with retrognathia in non growing individuals treatment and promotes a mandibular supplementary growth, but, due to the wide age range, absence of control group and number of individuals, results should be carefully analyzed and more studies, preferably Randomized Clinical Trials, are necessary to understand the mandibular behavior during JFO Class II with retrognathia treatment.
5. Conclusions
In the sample studied jaw functional orthopedics showed to be efficient to correct the overjet in class II non-growing patients.
Mandibular advancement with functional orthopedic appliances promotes a supplementary mandibular growth in non-growing patients
Further studies are necessary for a better comprehension of the subject such as Randomized Clinical Trials.
References
-
W. R. Proffit and H. W. Fields, Contemporary Orthodontics. St Louis: Mosby, 2000, pp. 475–487.
-
J. A. Mcnamara, “Components of class II malocclusion in children 8-10 years of age,” Angle Orthodontist, Vol. 51, No. 3, pp. 177–202, 1981.
-
B. Kaya and R. Uyar, “Influence on smile attractiveness of the smile arc in conjunction with gingival display,” American Journal of Orthodontics and Dentofacial Orthopedics, Vol. 144, No. 4, pp. 541–547, Oct. 2013, https://doi.org/10.1016/j.ajodo.2013.05.006
-
O. A. Pozza, R. H. Cançado, F. P. Valarelli, K. M. S. Freitas, R. C. Oliveira, and R. C. G. Oliveira, “Attractiveness of the facial profile: comparison of class II patients treated with Twin Force® or intermaxillary elastics,” Dental Press Journal of Orthodontics, Vol. 26, No. 5, 2021, https://doi.org/10.1590/2177-6709.26.5.e212014.oar
-
S. Paduano, R. Rongo, R. Bucci, G. Carvelli, and I. Cioffi, “Impact of functional orthodontic treatment on facial attractiveness of children with class II division 1 malocclusion,” European Journal of Orthodontics, Vol. 42, No. 2, pp. 144–150, Apr. 2020, https://doi.org/10.1093/ejo/cjz076
-
O. Almășan, A. Kui, I. Duncea, A. Manea, and S. Buduru, “Temporomandibular joint disk displacements in class II malocclusion and cervical spine alterations: systematic review and report of a hypodivergent case with MRI bone and soft tissue changes,” Life, Vol. 12, No. 6, p. 908, Jun. 2022, https://doi.org/10.3390/life12060908
-
C. Sandoval, A. Díaz, and G. Manríquez, “Relationship between craniocervical posture and skeletal class: A statistical multivariate approach for studying Class II and Class III malocclusions,” CRANIO®, Vol. 39, No. 2, pp. 133–140, Mar. 2021, https://doi.org/10.1080/08869634.2019.1603795
-
G. Zokaitė, K. Lopatienė, A. Vasiliauskas, D. Smailienė, and G. Trakinienė, “Relationship between Craniocervical Posture and Sagittal Position of the Mandible: A Systematic Review,” Applied Sciences, Vol. 12, No. 11, p. 5331, May 2022, https://doi.org/10.3390/app12115331
-
M. Watanabe, T. Yamaguchi, and K. Maki, “Cervical vertebra morphology in different skeletal classes. A three-dimensional computed tomography evaluation,” The Angle Orthodontist, Vol. 80, No. 4, pp. 719–724, Jul. 2010, https://doi.org/10.2319/100609-557.1
-
I. Klostermann, C. Kirschneck, C. Lippold, and S. Chhatwani, “Relationship between back posture and early orthodontic treatment in children,” Head and Face Medicine, Vol. 17, No. 1, pp. 1–8, Dec. 2021, https://doi.org/10.1186/s13005-021-00255-5
-
P. Planas, Reabilitação Neuro-Oclusal. (in Portugese), MEDSI, Médica e Científica, 1997.
-
P. Robin, “Observation sur un nouvel appareil de redressement,” Rev Stomatol, Vol. 9, pp. 423–32, 1902.
-
M. D. Austro-Martinez, A. I. Nicolas-Silvente, E. Velasco-Ortega, A. Jimenez-Guerra, and J. A. Alarcon, “Stability of class II malocclusion treatment with the Austro Repositioner followed by fixed appliances in brachyfacial patients,” International Journal of Environmental Research and Public Health, Vol. 18, No. 18, p. 9793, Sep. 2021, https://doi.org/10.3390/ijerph18189793
-
M. Alikhani et al., “Age-dependent biologic response to orthodontic forces,” American Journal of Orthodontics and Dentofacial Orthopedics, Vol. 153, No. 5, pp. 632–644, May 2018, https://doi.org/10.1016/j.ajodo.2017.09.016
-
T. El-Bialy, T. Shipley, and K. Farouk, “Effect of high-frequency vibration on orthodontic tooth movement and bone density,” Journal of Orthodontic Science, Vol. 8, No. 1, p. 15, 2019, https://doi.org/10.4103/jos.jos_17_19
-
S. Reiss et al., “Biomarkers of orthodontic tooth movement with fixed appliances and vibration appliance therapy: a pilot study,” European Journal of Orthodontics, Vol. 42, No. 4, pp. 378–386, Sep. 2020, https://doi.org/10.1093/ejo/cjaa026
-
M. Alikhani et al., “Vibration paradox in orthodontics: anabolic and catabolic effects,” PLOS ONE, Vol. 13, No. 5, p. e0196540, May 2018, https://doi.org/10.1371/journal.pone.0196540
-
D. González Espinosa, M. Santos, S. M. D. A. Mendes, and D. Normando, “Mandibular propulsion appliance for adults with Class II malocclusion: a systematic review and meta-analysis,” European Journal of Orthodontics, Vol. 42, No. 2, pp. 163–173, Apr. 2020, https://doi.org/10.1093/ejo/cjz089
-
A. T. Dibiase, L. Lucchesi, U. Qureshi, and R. T. Lee, “Post-treatment cephalometric changes in adolescent patients with Class II malocclusion treated using two different functional appliance systems for an extended time period: a randomized clinical trial,” European Journal of Orthodontics, Vol. 42, No. 2, pp. 135–143, Apr. 2020, https://doi.org/10.1093/ejo/cjz059
-
H. Mohammed, E. Čirgić, M. Z. Rizk, and V. Vandevska-Radunovic, “Effectiveness of prefabricated myofunctional appliances in the treatment of Class II division 1 malocclusion: a systematic review,” European Journal of Orthodontics, Vol. 42, No. 2, pp. 125–134, Apr. 2020, https://doi.org/10.1093/ejo/cjz025
-
D. R. Martins, G. R. P. Janson, R. R. Almeida, A. Pinzan, J. F. C. Henriques, and M. R. Freitas, de. Atlas de crescimento craniofacial. São Paulo: SANTOS, 1998.
-
A. K. Jena, R. Duggal, and H. Parkash, “Skeletal and dentoalveolar effects of Twin-block and bionator appliances in the treatment of Class II malocclusion: A comparative study,” American Journal of Orthodontics and Dentofacial Orthopedics, Vol. 130, No. 5, pp. 594–602, Nov. 2006, https://doi.org/10.1016/j.ajodo.2005.02.025
-
W. A. Simões, Ortopedia Funzionale Dei Mascellari Attraverso La Riabilitazione Nuero-Occlusale. (in Italian), Orbetello, 2010.
-
P. C. Riddle et al., “Mechanobehavior and mandibular ramus length in different facial phenotypes,” The Angle Orthodontist, Vol. 90, No. 6, pp. 866–872, Nov. 2020, https://doi.org/10.2319/032420-217.1
-
R. G. Behrents, Growth in the Aging Craniofacial Skeleton. Monograph 17. Craniofacial Growth Series. Michigan University, Center for Huan Growth and Development, 1985.
-
O. Santiago Júnior, M. V. Lucas Ferreira, and R. Huebner, “Treatment of temporomandibular dysfunction with jaw functional orthopedics: a retrospective study,” Jaw Functional Orthopedics and Craniofacial Growth, Vol. 1, No. 1, pp. 18–27, Jun. 2021, https://doi.org/10.21595/jfocg.2021.22080
-
A. G. Petrovic, J. J. Stutzmann, and J. Lavergne, “Efeito dos aparelhos funcionais sobre a cartilagem do côndilo mandibular,” (in Portuguese), Ortodontia, pp. 64–81, 1991.
-
Rabie Ab, Leung Fy, Chayanupatkul A., and Hägg U., “The correlation between neovascularization and bone formation in the condyle during forward mandibular positioning,” The Angle Orthodontist, Vol. 72, No. 5, pp. 431–438, Oct. 2002, https://doi.org/10.1043/0003-3219(2002)072
About this article
The authors have not disclosed any funding.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
The authors declare that they have no conflict of interest.
All individuals treated (or theirs tutors) signed a consent form to use the data obtained with their treatment for didactic and scientific purpose. According to item V of the sole paragraph of resolution No. 510/2016 in its article 1st – “investigation with data base, whose information is aggregated, without the possibility of individual identification”, there is no need for approval of the research by the ethics committee (https://www.propq.ufscar.br/etica/cep/duvidas-frequentes).

