Abstract
The aim of the research is to observe whether specific developmental disorder of motor function (SDDMF) in infancy affects 6-7 years old children’s balance and to find out does physiotherapy (PT) is beneficial for enhancing and maintaining this feature. The study involved 97 right-hand 6-7 years old children. Participants were divided into two groups: study and control group. In the study group, there were children who had SDDMF in infancy being 4-11 months old and participated in a PT program in infancy. Control group participants didn’t have SDDMF and PT in infancy. The balance was assessed using a computerized balance platform. The study group had 16 physiotherapy procedures. A data analysis showed significant differences of participants’ balance characteristics in frontal and sagittal planes: comparing study and control group results before PT in open eyes with feedback performance. There was a significant difference of balance between the study group before and after a PT with the control group when participants performed tasks with open eyes without a feedback. SDDMF in infancy affects 6-7 years old children’s balance and PT is beneficial for enhancing and maintaining these features for 6-7 years old children.
1. Introduction
Gross motor function is the process of developing from head to legs; after a child is able to keep his head upright and control the shoulder muscles and trunk, the child will be able to control his or her legs [1, 2]. Fine motor function develops from proximal to distal direction. For example, if the child is unable to control his trunk or shoulder line, he or she will not be able to manage hand and finger movements [3]. Each new motor skill is acquired in a specific order that is dependent on that which has been developed earlier; for example, first a child learns to support his or her body weight, then that child will begin to stand and later walk. It’s very important to learn all the movements from the beginning; it is the basis for all other, more complex movements [1, 2].
In Lithuania, the specific developmental disorder of motor function (SDDMF) diagnosed in infants has been tracked for several years. In 2006, 3,039 babies were diagnosed; in 2007, 3,692 babies; in 2008, 4,017 babies; in 2009, 4,237 babies; in 2010, 4,753 babies; in 2011, 4,527 babies; and in 2012, 4,088 babies.
According to the ICD-10 (2016): Specific developmental disorder of motor function (SDDMF) is defined as a “disorder in which the main feature is a serious impairment in the development of motor coordination that is not solely explicable in terms of general intellectual retardation or of any specific congenital or acquired neurological disorder. Nevertheless, in most cases, a careful clinical examination shows marked neurodevelopmental immaturities such as locomotor movements of unsupported limbs or mirror movements and other associated motor features, as well as signs of impaired fine and gross motor coordination” [4]. The SDDMF is characterized by a 2-3-month motor delay [5].
Motor development depends on child’s genetics, gender, environmental stimulation and the child’s personal motivation. Very often, same-age children’s motor skills may vary but motor development patterns are universal and common to children in general [6].
Many authors argue that preschool and early school age is the primary sensory and motor development phase for children, in which the focus should be on the motor system, which directly affects all other systems’ development. It is a critical period for a child’s basic motor development [6-8].
Some authors note that the basic motor movements develop from the second year until the seventh years of age [9, 10]. However, the specific motor abilities are acquired in the seventh through the eleventh years of life [11]. During this period, additional movement skills are developed, particularly those which are important for daily and sports activities [12].
Between ages of two and seven, children are learning and improving their balance skills in a variety of conditions. The most important motor skills, such as standing, standing on one leg, walking, walking on the balance beam, running, jumping, throwing, and catching, are acquired in three phases [9, 10]. The first phase is when the child tries to perform movements without good coordination or control. In the second phase, motor control and coordination are much better. This occurs in children of around 3-4 years old. The last phase is the maturity phase – here, the movements are already sufficiently controlled and coordinated. Most 5 and 6-year-old children should already have reached the maturity phase [9].
The balance is very important in the preschool and early school age when children begin to act consciously and purposefully control their movements. The ability to integrate information from visual, vestibular, and proprioception systems, as well as the ability to select the proper muscles so that, during movement, the body mass centre is in the proper position, are very important for the body balance [13].
Because of motor function development, we chose 6 and 7-year-old children for our research. At this age, children start to spend more time sitting than walking. These children start going to school, and more than 6 hours per day are sitting at a table when, before that time, they were more frequently running, walking, and playing outside.
The aim of our research is to observe whether the specific developmental disorder of motor function in infancy affects 6 and 7-year-old children’s balance, and to find out whether physiotherapy (PT) is beneficial for enhancing and maintaining balance skills. SDDMF in infancy is adjusted very well by physiotherapy [14]. However, there are a lack of studies focused on whether SDDMF in infancy leads to balance disorders among 6 and 7-year-old children.
2. Methods
2.1. Study design
The study involved 97 right-hand 6- to 7-year-old children living in Kaunas (Lithuania). The study was performed in the Lithuanian University of Health Sciences, Institute of Sports.
2.2. Participants
Participants were divided into two groups: study and control group. In the study group, there were 6- to 7-year-old children who had the SDDMF in infancy being 4-11 months old and participated in a PT program in infancy. During this study, participants of the study group were tested two times – before and after physiotherapy. After the first assessment, the study group participants had 16 physiotherapy procedures, at a frequency of twice a week. During this PT program, children didn’t have physiotherapy with any other physiotherapist. All of them participated in some form of exercise or sports in school; however, they didn’t start any new physical activities during the participation in the study.
The control group was made up of 6- or 7-years-old children, who didn’t have SDDMF [15] in infancy. In infancy, these children didn’t need or have physiotherapy, and their motor function was checked by a general practitioner or paediatrician. The control group participants underwent the same tests as the study group on one-time basis, and didn’t receive physiotherapy at this time.
2.3. Inclusion and exclusion criteria
2.3.1. Inclusion criteria
Study group – 6- to 7-year-old right-hand children who had SDDMF between 4-11 months old. As infants, all these children had 16 physiotherapy procedures, which were conducted at a frequency twice a week. The evaluation (before and after physiotherapy) was done using a certified assessment scale: Munich Functional Developmental Diagnostics [16, 17]. After the physiotherapy program, the motor delay of all participants disappeared, and motor development matched the child’s age. The study group participants had a good or average posture score. Control group – 6- to 7-year-old right-hand children who didn’t have SDDMF in infancy. The control group participants had a good or average posture.
2.3.2. Exclusion criteria
For both groups – 6- to 7-year-old left-hand children; participants who had excellent, moderate, or poor posture score were excluded from the study; participants who had other motor development disorder in infancy or till 7 years of childhood.
2.4. Intervention
Physiotherapy for infants was conducted according to the infant’s age by physiotherapist. The aim is to teach and to develop correct movement during active movements: crawling, sitting, walking, grasping.
Physiotherapy for 6- to 7-year-old children was active; with small and big balls; with jumping cord; a lot of hops; standing on one foot; walking on the toes and heels and etc. The aim for the study group physiotherapy was to improve balance, posture, and gross motor function.
2.5. Outcomes and measurements
The posture of all participants was assessed using a W. W. K. Hoeger scale. Many researchers are using this visual posture assessment scale [18]. This method is an easy way to assess posture – any participant with perfect posture of a specific region is awarded 5 points; in case of a small deviation from the norm, 3 points, and if a large deviation from the correct posture is observed, 1 point. There are 10 evaluation criteria: in the frontal plane – position of the head, shoulder height, position of the spine, pelvis, knees and ankles; and in the sagittal plane – position of the neck and upper spine, trunk, belly, the lower part of spine and legs. The various posture categories are determined according to the sum of the ratings obtained for each body segment. Posture evaluation standards: more than 45 points – posture is excellent (maximum is 50); 40-44 points – good; 30-39 points – average; 20-29 points – moderate; less than 19 points – poor posture [18]. All the participants had a good or average posture score. Participants who didn’t have good or average posture per the W. K. Hoeger scale were excluded from the study. The posture was chosen as criteria for inclusion in the study because it’s known that posture can affect the balance [19].
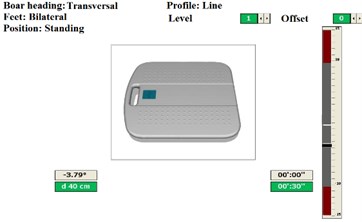
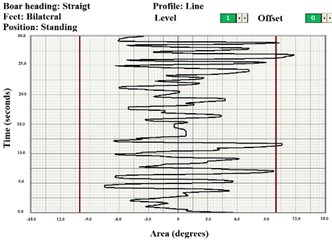
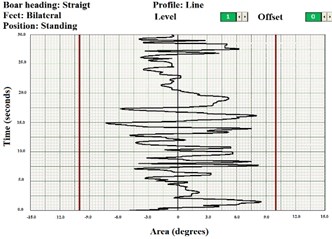
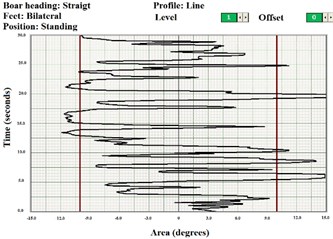
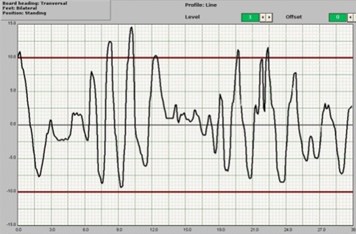
The balance was assessed using a computerized balance platform (Italy, 2002, 93/42/CEE). The system consists of a 42×42 cm platform, computer, and computer system. Each participant performed 6 exercises on this platform. Testing took 3 minutes for each participant. Each of the 6 tests lasted 30 seconds. The balance was evaluated in both the frontal (Fig. 1(a)) and sagittal (Fig. 1(b)) planes while the participant was standing. The first 3 tests were taken in the sagittal plane, and the other 3 tests – in the frontal plane. The first and fourth tests were conducted with a feedback – children saw the white small line in the computer screen and tried to hold black small line on it. The aim is to be as straight as possible. The second and fifth tests were taken in different planes without a feedback (Fig. 2). For the third and sixth tests, participants performed with closed eyes. All these tests were taken standing with straight knees, as the requirement for participants was: don’t bend the knees. All movements should be fixed in one body segment – hips [20].
Fig. 1Computer screen while children took the first and fourth tests
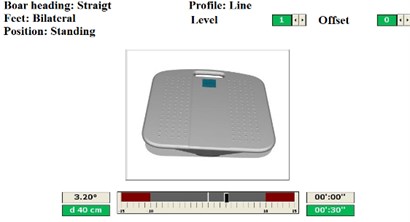
a) Frontal plane
b) Sagittal plane
Fig. 2Computer screen while children took the second and fifth tests
Accumulated data were processed by the computer program. Exercise performance was measured on the right and left: total area [sec], external area [sec], external time [sec], recovery time [sec] (Fig. 3). From these four numbers, the summative assessment (Fig. 4) was evaluated (ranging from 0 to 100). A lower value of summative assessment means better balance. Total score was calculated using a software algorithm, comparing the left and right side of the body – deviation from the midline of the results. It is also called as the stability index, it is based on the weighted average of all the variables, where 100 denotes the weakest stability and 0 the best one. The algorithm of summative assessment (stability index) calculation is (total area (left) + total area (right) + external are (left) + external area (right) + external time (left) + external time (right) + recovery time (left) + recovery time (right))/8.
2.6. Statistical analysis
The difference between two independent groups was tested using Mann-Whitney U test. While the difference before and after physical therapy was calculated using Wilcoxon matched pairs rank test. Nonparametric tests were used because that research data based on fewer assumptions – they do not assume that the outcome is approximately normally distributed. The significance level p<0.05 was used for the verification of statistical hypotheses. Data are presented as median (xme), first quartile (Q1) – third quartile (Q3) and mean (ˉx) – xme(Q1-Q3; ˉx).
2.7. Ethics statement
This study was approved by the Lithuanian Regional Biomedical Research Ethics Committee. Written informed consent was obtained from all participants’ parents/guardians.
3. Results
3.1. Participant recruitment
Study group. Forty-four children (21 boys and 23 girls) who had SDDMF in infancy were involved in the first testing, but only 35 participants (17 boys and 18 girls) finished this study, and as such, were tested the second time.
It is important to note that the assessment of the study group’s participants (n=363) was conducted when the participants were between 4-11 months old. All children had SDDMF in this age. Only 333 infants finished the physiotherapy program and had one more motor development assessment. After 6 or 7 years, we reached 109 parents and asked them to bring their children for the assessment again. Of the 109 parents, only 44 agreed to participate in our study.
Control group. There were 53 children who didn’t have SDDMF in infancy – 25 boys and 28 girls – in the control group. Baseline characteristics are in 1st table.
3.2. Baseline characteristics
Table 1Body height and weight of the participants
Height (cm) | Weight (kg) | |||||
Group | Min | Max | Average ±SD | Min | Max | Average ±SD |
Study | 116 | 141 | 128.6±6.0 | 18.2 | 36.9 | 24.9±5.6 |
Control | 117 | 140,5 | 129.5±7.4 | 18.4 | 37.9 | 24.8±5.3 |
3.3. Outcomes
3.3.1. Frontal plane
Before physiotherapy, we noticed that control group’s summative assessment of stability index was lower than study group in exercises with open eyes (Table 2) (Test criteria – Tables A1-A3). It means that, in the frontal plane, the control group’s participants’ balance was better while they took an exercise with open eyes. After the physiotherapy program, we noticed no statistically significant difference between the control and study group results while performing open eyes exercise with feedback test. There is no significant difference comparing closed eyes exercise of the study group before and after physiotherapy and control group results. Study group results after the physiotherapy program were better in all three tests (p<0.05).
The exercise performance with closed eyes was completed with the worst result of study group before and after physiotherapy. There was no significant difference while the study group before and after physiotherapy took both performance with open eyes in the frontal plane. The analysis of control group results demonstrated that there was a statistically significant difference between all three performances (Fig. 5).
Table 2Median, first quartile – third quartile and mean of study group before and after physiotherapy and control group stability index results of frontal plane
Open eyes with feedback | Open eyes without feedback | Closed eyes | |
Study group before PT | 20.9 (15.7/29.6; 23.2) | 23.1 (18.6/27.4; 24.0) | 42.0 (35.9/45.9; 41.1) |
Study group after PT | 15.1 (12.3/21.9; 17.4) | 16.7 (15.3/21.8; 18.9) | 38.2 (31/44.7; 37.8) |
Control group | 15.6 (12.9/21.4; 17.6) | 12.8 (10.0/19.7; 15.0) | 41.6 (35.4/45.0; 40.4) |
Comparing how many degrees per second participants stay in the left or right side (Table 2), we noticed that before and after physiotherapy and the control group participants stayed in the right side more than in the left side while taking an exercise with open eyes with a feedback and without a feedback (p<0.05) (Fig. 6). We didn’t get any significant differences between staying in the right and left in the exercise with closed eyes (Test criteria – Table A4-Table A6).
Fig. 5Comparison of children stability index results for study group children before and after physiotherapy and control group children, in frontal plane (a, b, c, d, e, f, g, h, i identification of column – p< 0.05)
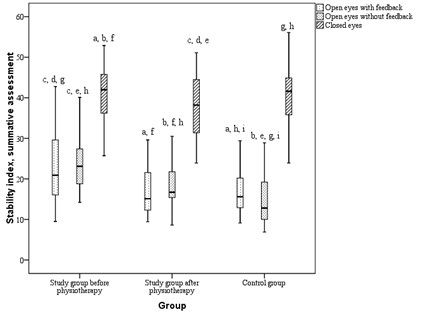
Table 3Median, first quartile – third quartile and mean of study group before and after physiotherapy and control group results of staying in right or left (degrees per seconds)
Open eyes with feedback | Open eyes without feedback | Closed eyes | ||||
Right | Left | Right | Left | Right | Left | |
Study group before PT | 82.9 (66.5/110.9; 89.4) | 62.6 (49.4/99.6; 73.7) | 97.5 (72.7/118.3; 94.2) | 74.7 (38.3/94.6; 72.1) | 133.8 (108.1/161.1; 134.3) | 128.5 (91.6/160.3; 129.1) |
Study group after PT | 66.5 (47.2/94.3; 74.2) | 49.0 (37.7/60.2; 52.3) | 83.6 (48.8/111.3; 80.2) | 52.1 (31.3/80.7; 58.5) | 129.7 (90.5/174.3; 131.3) | 107.8 (86.1/130.9; 111.9) |
Control group | 64.1 (47.0/82.2; 71.2) | 53.2 (38.3/71.2; 58.1) | 58.9 (48.2/87.1; 67.3) | 40.8 (27.0/65.5; 135.5) | 134.2 (112.25/153.9; 122.2) | 126.5 (102.1/152.9; 42.2) |
Fig. 6Fluctuation while children took performance in frontal plane
a) With feedback
b) Without feedback
c) Closed eyes
3.3.2. Sagittal plane
The control group results were better than the study group results before and after physiotherapy while they took an exercise with open eyes without feedback (Table 4). There is no statistically significant difference while they took open eyes with feedback performance. The study group results while performing exercise with closed eyes were statistically significant better than the control group results in the sagittal plane after physiotherapy. After the physiotherapy program, we noticed no statistically significant difference while performing open-eyes exercises. There was a significant difference after physiotherapy just in closed eyes exercise (Test criteria – Table A1-Table A3).
The analysis of study group before and after, and control group results demonstrated that there was a statistically significant difference between all three performances (Fig. 7).
Fig. 7Comparison of children stability index results for study group children before and after physiotherapy and control group children, in sagittal plane (a, b, c, d, e, f, g, h, i identification of column – p< 0,05)
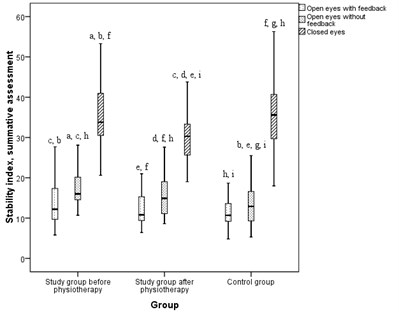
Table 4Median, first quartile – third quartile and mean of study group before and after physiotherapy and control group stability index results of sagittal plane
Open eyes with feedback | Open eyes without feedback | Closed eyes | |
Study group before PT | 12.2 (9.7/18.2; 16.4) | 16.0 (14.2/20.6; 17.4) | 33.8 (30.3/42.4; 36.5) |
Study group after PT | 10.8 (9.3/15.4; 12.4) | 14.9 (10.9/19.2; 15.8) | 30.3 (25.6/33.3; 31.6) |
Control group | 10.7 (9.2/13.8; 11.5) | 12.9 (9.3/16.7; 13.5) | 35.6 (29.7/41.0; 35.5) |
Comparing how many degrees per second participants stayed forward and backwards, we noticed that before physiotherapy, the study group participants stayed forward more than backwards while took an exercise with closed eyes (Table 5) (p<0.05) (Fig. 8). After physiotherapy, we didn’t get any differences. The control group participants stayed more backwards while tooking an exercise with open eyes without feedback and more forward in an exercise with closed eyes.
Observing the differences between the groups – if some participants of the group moving more to the right or left, we noticed that study groups results before physiotherapy were different from the control group ones – in the frontal plane, the study groups participants stayed more in the left or right than the control group ones. The study group participants were more unstable before physiotherapy than the control group ones. When comparing the study group data after physiotherapy with the control group, this difference disappeared – both groups stayed the same area in the left or right. There is no significant difference in staying forward or backwards comparing study group results before and after physiotherapy with control group results (Test criteria – Table 6-Table 8).
Table 5Median, first quartile – third quartile and mean of study group before and after physiotherapy and control group results of staying in forward and backwards (degrees per seconds)
Open eyes with feedback | Open eyes without feedback | Closed eyes | ||||
Forward | Backwards | Forward | Backwards | Forward | Backwards | |
Study group before PT | 47.0 (23.7/68.2; 55.3) | 48.5 (37.3/60.6; 51.0) | 63.5 (36.4/85.2; 66.7) | 54.9 (38.9/96.4; 65.4) | 134.2 (92.2/186.5; 141.6) | 82.7 (53.5/118.5; 89.8) |
Study group after PT | 41.5 (27.2/57.6; 44.8) | 45.7 (32.1/61.8; 50.1) | 45.2 (25.3/65.3; 50.6) | 65.7 (40.0/85.8; 70.3) | 116.1 (79.1/165.7; 118.5) | 93.0 (47.5/133.4; 90.4) |
Control group | 38.8 (24.9/55.4; 42.2) | 42.9 (33.8/56.8; 47.5) | 38.2 (18.7/55.5; 43.1) | 55.2 (33.1/85.0; 61.5) | 117.4 (96.25/164.6; 138.5) | 96.1 (64.0/131.1; 94.9) |
Fig. 8Fluctuation while children took exercise in sagittal plane
a) With feedback
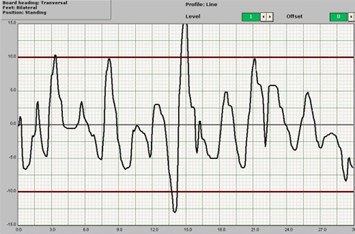
b) Without feedback

c) Closed eyes
4. Discussion
To evaluate the balance, we used a balance platform. To keep body straight in line, good coordination between the muscles and nervous system is essential. The ability to maintain balance is disturbed if any part of the system responsible for the balance does not work properly [21, 22]. We noticed in our research that the specific developmental disorder of motor function in infancy can affect 6-7 years old children balance.
Impaired motor development combines posture, upper limbs and head control, as well as determines their daily activities and achievements [23].
Some authors studied the torso muscles activity during voluntary movements of the hands in healthy children and children with SDDMF. The researchers found that children with developmental disorders included abnormal muscle activation, activated muscles and recovered more slowly. Also these children were slower to respond to stimuli. It was concluded that children with impaired muscle activation had the disturbed balance, posture and upper limb coordination [13]. In our research, we noticed that children who had specific developmental disorder of motor function in infancy had the worst balance than children without specific developmental disorder of motor function in infancy.
It is very important to evaluate posture and balance in childhood. After the examination of balance, it is very important to train it because of some motor abilities, such as running; jumping may be adversely affected if an early age balance is insufficiently studied. Also in case of bad balance children are more likely to suffer injury in daily or sports activities [24].
Long-term studies have shown that preschools children who can boast great motor abilities, often experience anxiety in later of life and may have emotional problems [25]. This idea could be the subject of our future research.
5. Conclusions
There are less significant differences performing balance exercises with open eyes with and without feedback after physiotherapy between children who had and didn’t have specific developmental disorder of motor function in infancy than before physiotherapy.
This research showed that there is better balance after physiotherapy for 6-7 years old children who had specific developmental disorder of motor function in infancy. These children before physiotherapy stayed in the right side and backwards more than in the left side and forward. After physiotherapy, we didn’t get any significant differences in these positions.
References
-
Martens R., Hurks P. P. Jolles J. Organizational strategy use in children age 5-7: standardization and validity of the Rey Complex Figure Organizational Strategy Score (RCF-OSS). The Clinical Neuropsychologist, Vol. 28, Issue 6, 2014, p. 954-73.
-
Casas M., Chatzi L., Carsin A. E., et al. Maternal pre-pregnancy overweight and obesity, and child neuropsychological development: two Southern European birth cohort studies. International Journal of Epidemiology, Vol. 42, Issue 2, 2013, p. 506-17.
-
Rheim M., Buchmann A., Hagmann C., et al. Brain volumes predict neurodevelopment in adolescents after surgery for congenital heart disease. Brain: A Journal of Neurology, Vol. 137, Issue 1, 2014, p. 268-76.
-
Definition, Diagnosis, Assessment and Intervention of Developmental Coordination Disorder (DCD). EACD Recommendations, 2011.
-
World Health Organization International Classification of Diseases. http://www.icd10data.com/ICD10CM/Codes/F01-F99/F80-F89/F82-/F82, 2015.
-
Cools W., Martelear K., Samaey C. H., et al. Movement skill assessment of typically developing preschool children: a review of seven movement skill assessment tools. Journal of Sport Science and Medicine, Vol. 8, 2009, p. 154-168.
-
Hardy L. L., King L., Farrell L., et al. Fundamental movement skills among Australian preschool children. Journal of Science and Medicine in Sport, Vol. 5, Issue 13, 2009, p. 503-508.
-
Živčić K., Trajkovski-Višić B., Sentderdi M. Changes in some of the motor abilities of preschool children (age four). Physical Education and Sport, Vol. 6, Issue 1, 2008, p. 41-50.
-
Foulkes J. D., Knowles Z., Fairclough S. J., et al. Fundamental movements skills of preschool children in Northwest England. Perceptual and Motor Skills, 2015.
-
Foweather L., Knowles Z., Ridgers N. D., et al. Fundamental movement skills in relation to weekday and weekend physical activity in preschool children. Journal of Science and Medicine in Sports, Vol. 18, Issue 6, 2015, p. 691-6.
-
Clark J. E. On the problem of motor skill development. Journal of Physical Education, Recreation and Dance, Vol. 78, Issue 5, 2007, p. 39-43.
-
Sun S. H., Shu Y. C., Shih et al. C. L. Development and initial validation of the preschooler gross motor quality scale. Research in Developmental Disabilities, Vol. 31, Issue 6, 2010, p. 1187-96.
-
Shickedanz J. A. Understanding Children and Adolescents. Allyn and Bacon, Boston, 2001, p. 285-297.
-
Weber P., Jenni O. Screening in child health: studies of the efficacy and relevance of preventive care practices. Deutsches Arzteblatt International, Vol. 109, Issue 24, 2012, p. 431-435.
-
World Health Organization International Classification of Diseases. http://www.who.int/classifications/icd/en/, 2015.
-
Antonini U., Soldini E. A., D’Apuzzo V., et al. Longitudinal neurodevelopmental evolution in children with severe non-progressive encephalopathy. Brain and Development, Vol. 35, Issue 6, 2013, p. 548-54.
-
Koum L., Werner-Spangenberg I., Saling E. Early child morbidity and late development following primary abdominal cesarean section in breech presentation near term. Geburtshilfe und Frauenheilkdunde, Vol. 46, Issue 9, 1986, p. 609-18.
-
Hoeger W. K. W., Hoeger A. S. Principles and Labs for Fitness and Wellness. 12 Edition, 2014.
-
Adolph K. E., Tamis-Lemonda C. S., Ishak S., et al. Locomotor experience and use of social information are posture specific. Developmental Psychology, Vol. 44, Issue 6, 2008, p. 1705-14.
-
Tchórzewski D., Bujas P., Jankowicz-Szymańska A. Body posture stability in ski boots under conditions of unstable supporting surface. Journal of Human Kinetics, Vol. 38, 2013, p. 33-44.
-
Szczepanowska-Wolowiec B., Drzal-Grabiec J., Sztandera P., et al. Parameters of dynamic balance in the frontal and sagittal plane and their correlations with poor postures in children aged 10-12 from the Maslow district in Swietokrzyskie province. Studia Medyczne, Vol. 29, Issue 4, 2013, p. 308-313.
-
Vandendriessche J. B., Vandorpe B., Coelho-e-Silva M. J., et al. Multivariate association among morphology, fitness, and motor coordination characteristics in boys age 7 to 11. Pediatric Exercise Science, Vol. 23, Issue 4, 2011, p. 504-520.
-
Bair W., Kiemel T., Jeka J. J., et al. Development of multisensory reweighting is impaired for quiet stance control in children with developmental coordination disorder (DCD). PLoS ONE, Vol. 7, Issue 7, 2012, p. 1-18.
-
Mickle K. J., Munro B. J., Steele J. R. Gender and age affect balance performance in primary school – aged children. Journal of Science and Medicine in Sport, Vol. 14, Issue 3, 2011, p. 243-248.
-
Piek J. P., Barrett N. C., Smith L. M., et al. Do motor skills in infancy and early childhood predict anxious and depressive symptomatology at school age? Human Movement Science Vol. 29, 2010, p. 777-786.
-
Health Statistics of Lithuania. Hygiene Institute, http://sic.hi.lt/html/lss.htm, 2015.
-
Johnston L. M., Burns Y. R., Brauer S. G., et al. Differences in postural control and movement performance during goal directed reaching in children with Developmental Coordination Disorder. Human Movement Science, Vol. 21, 2002, p. 583-601.
About this article
Margarita Radžiūnienė did an experiment, analysis of results, discussion, conclusions; Vilma Mauricienė wrote an introduction, small part of analysis of the results, discussion, conclusions; Kristina Berškienė did statistical analysis; Giedrius Vanagas create research methodology; Kęstutis Radžiūnas helped to do an experiment.

