Abstract
Cardiovascular diseases are the leading cause of death globally accounting for 32 % of all global deaths. Addressing modifiable risk factors, including hypertension and stress, remains paramount in the prevention of CVD. This study aimed to assess the impact of the balneotherapy on blood pressure, heart rate, electrocardiogram parameters, utilization of antihypertensive medications, and stress levels. Methodology. Multicenter randomized controlled single-blind parallel group trial was made in 6 Lithuania resort centers. 373 participants with the stress level > 3 (10, VAS) randomly divided into 6 groups in two clusters for receiving a 6- or 11-day complex treatment using natural resources – mineral waters, peloids, salt, nature therapy; follow-up period was 6 months. The BP, HR, ECG, stress level and other parameters were analyzed in 131 participants who passed a full course of investigation. Results. The significant reduction of systolic blood pressure after treatment (7.8 mmHg) and during 6 months (7.3 mmHg) together with diastolic 5.5 after 6 month and heart rate (4 b/min) was achieved in 11-day ambulatory balneotherapy group. Increase in the activity of the parasympathetic nervous system was observed, which is reflected by an increase in the duration of the ECG indicators. The stress level decreased by up to 43%, and stress management improved by up to 41% following inpatient treatment. Conclusion. Therapy using natural resources could stand for additional cardiovascular disease prevention and management method in integrative therapy.
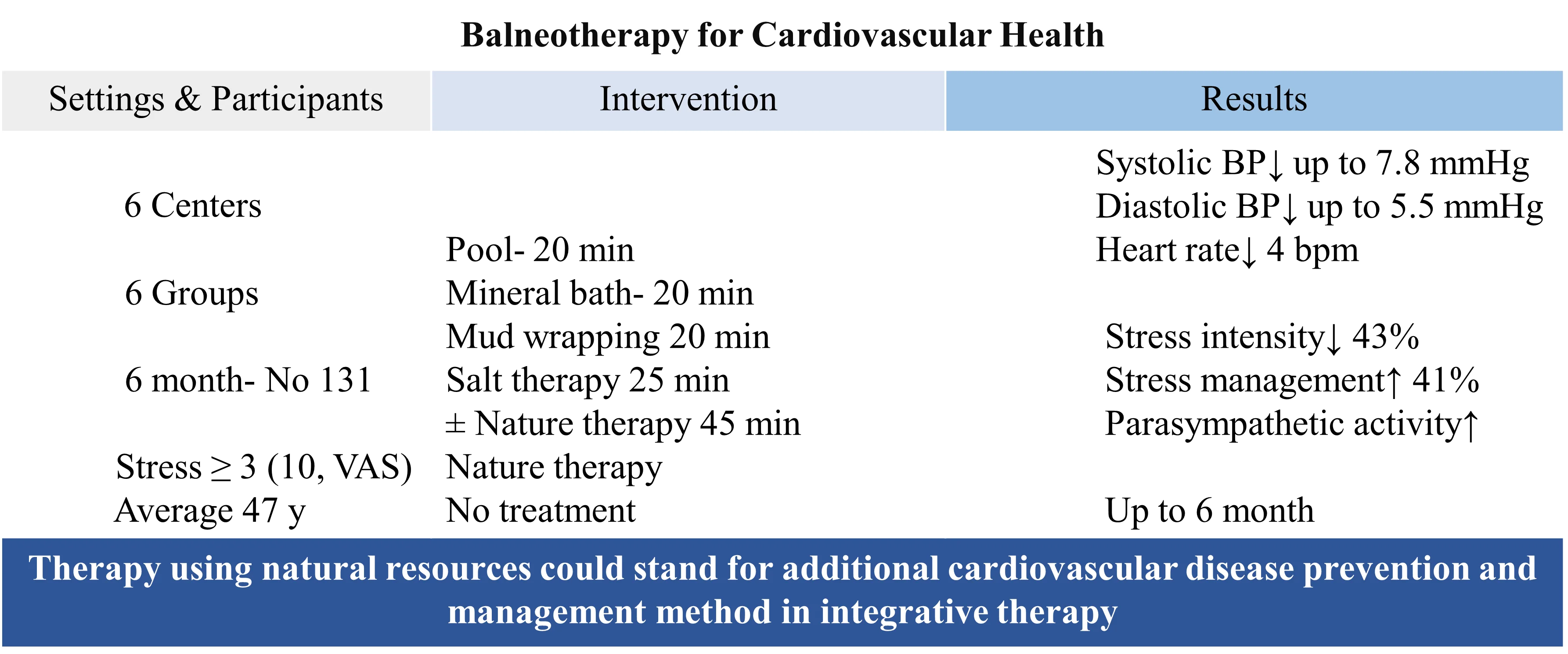
Highlights
- Cardiovascular diseases rank as the leading cause of mortality worldwide, accounting for a staggering one-third of all global deaths highlighting the need for effective prevention strategies.
- A two-week balneotherapy regimen has demonstrated notable efficacy in reducing key cardiovascular indicators. Systolic blood pressure saw a remarkable decrease of 8 mmHg, while heart rate experienced a notable decline of 4 beats per minute, accompanied by a tangible reduction in stress level.
- By integrating balneotherapy into the management protocols for individuals with or at risk of cardiovascular conditions, healthcare practitioners can potentially offer more comprehensive and tailored treatment approaches.
1. Introduction
Cardiovascular diseases (CVD) are the leading cause of death worldwide accounting for 32 % of all global deaths (2020) with big increase of 18.7 % from 2010, and a major contributor to disability [1]. According to data from the Lithuanian Hygiene Institute, in 2022, diseases of the circulatory system accounted for the majority, constituting 52.5 % (22,503 annual) of all deaths in the statistics [2]. CVD can be caused by a combination of socioeconomic, metabolic, behavioral, and environmental risk factors, including high blood pressure, unhealthy diet, high cholesterol, diabetes, air pollution, obesity, tobacco use, kidney disease, physical inactivity, harmful use of alcohol and stress [3].
One of greatest modifiable risk factors of CVD including heart failure, stroke, valvular heart diseases, cardiac arrhythmias, and heart attack is hypertension producing also substantial adverse economic and social impacts. The prevalence of hypertension in different European countries accounts for 30-45 % of the general population [4], less than half of adults (42 %) with hypertension are diagnosed and treated [5], and only about 1 in 4 (24 %) have their condition under control [1]. Numerous clinical trials have shown that lowering blood pressure (BP) reduces CVD risk by 20 %-25 % for myocardial infarction, 35 %-40 % for stroke and by 50 % for heart failure [6]. Evidence suggests that heart rate (HR) is an independent risk factor for CVD and total mortality in patients with hypertension [7]. Electrocardiography (ECG) can also be used to detect patterns of ventricular overload to indicate more severe risk, ischemia, conduction defects, and arrhythmias [8]. While it is acknowledged that individuals experiencing high levels of distress face an elevated risk of conditions such as peripheral vascular disease, heart failure, coronary death, or incident non-fatal myocardial infarction, the significance of psychological stress as a risk factor for cardiovascular disease is frequently underestimated [9], [10].
Despite advances in medical treatment and interventions, addressing modifiable risk factors remains crucial in preventing CVD. To improve cardiovascular health globally, tailored innovative research approaches are necessary, focusing on inclusivity and holistic strategies. Both pharmacological and non-pharmacological methods, including lifestyle changes such as dietary interventions, weight management, tobacco cessation, physical activity, and stress management, have proven effective in reducing blood pressure and cardiovascular risk [11], [12]. Moreover, recognizing the protective role of positive psychological well-being against adverse health outcomes, including CVD, is essential [13]. In recent years, there has been a growing interest in exploring the potential of natural resources [14]. Balneotherapy (BT), a centuries-old practice utilizing mineral/geothermal water, peloids, and gases to improve health and alleviate symptoms, has garnered attention for its potential cardiovascular benefits via reducing cardiac workload and vasodilation effects [15]. Studies suggest that BT may lower BP, improve endothelial function and heart rhythm, and alleviate symptoms of cardiovascular conditions [16-21]. Its mechanism of action involves a complex synergistic combination of neuroendocrine and immunological effects, influenced by mechanical, thermal, chemical, and immunological factors [22], [23]. Spa resort treatments induce changes in the autonomic nervous system, reducing sympathetic activity and enhancing parasympathetic function [24]. However, further research is warranted to elucidate BT’s mechanisms of action, effects on different body systems, and optimize treatment protocols, as balneotherapy may represent a promising strategy for cardiovascular risk reduction and health promotion. Investigation of the impact of BT on key risk factors of CVD may uncover novel insights into its mechanisms of action and its potential as an adjunctive or alternative non-pharmacological and holistic therapy for individuals at risk of cardiovascular disease.
The aim of the study was to evaluate the effect of BT complex on BP, HR, ECG parameters, antihypertensive usage, and stress.
2. Materials and methods
2.1. Study design
Multicenter randomized controlled single-blinded (for researchers) parallel groups interventional study was made in Lithuania during period of January-September, 2023 in 6 medical spa centres Gradiali (Palanga), Atostogų parkas (Kretingos reg), Eglė (Druskininkai), Draugystė (Druskininkai), Tulpė (Birštonas), Versmė (Birštonas).
2.2. Participants
The inclusion criteria into study were age of 18-65 years, the intensity of stress 3 and more (10, VAS). The exclusion criteria: uncontrolled/decompensated systemic diseases (hematological, endocrine, rheumatological, renal, cardiovascular, digestive, pulmonary), active infection, malignant tumors, surgery or major trauma in the past year, applied balneotherapy treatment during a 3-month period, pregnancy/lactation, bleeding, severe mental and physical health problems. 373 persons meet eligibility criteria, were allocated to Klaipėda and Druskininkai clusters, coded by statistician and randomly assigned to the respective group (1-6) by a computer program after the initial examination (T0) at the study centers. Grouping was done by a statistician. The researchers conducting the clinical trial did not knew which group the subject belongs to. All the participants signed the informed consent with the information about the study aim, terms, and description of this study before it started. 346 participants received intervention. Four groups/arms (1-4) of participants received a 6 or 11-day BT complex treatment using natural resources – mineral waters, peloids, salt, nature therapy procedure, 5th group received nature therapy procedure alone, 6th was control group without treatment. 131 participants with complete data during six months period were selected for analysis of the effect on cardiovascular risk parameters.
2.3. Study outcomes and research tools
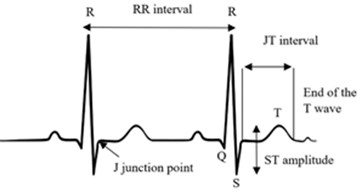
The primary study outcomes were effect on systolic (SBP) and diastolic (DBP) BP; secondary-effect on HR, ECG parameters RR, QRS, JT, stress intensity level was measured at baseline (T0), post-treatment (T1), 3-month follow-up (T2), 6-month follow-up period (T3). Systolic, diastolic BP, and HR were measured with automatic blood pressure monitor ADC Advantage 6021N; ECG – with LUMED® ECG Manager, digital 6 channels; stress intensity and management- visual-analogue scale (1-10) where for stress intensity 1 score was rated as no stress, 2-3 – low, 4-6 –medium, 7-9 – high, 10 – unbearable stress; for the stress management value 1 score was rated as does not manage stress at all, 2-3 manage it poorly, 4-6 – moderately, 7-9 – well, 10 – extremely well. ECG: we examined 3 indicators of ECG signals (Fig. 1) [25]:
– RR interval, measured in ms, is the interval between two adjacent R – the time interval between two heart contractions. The RR interval is determined by the intrinsic properties of the sinus node as well as autonomic influences, affected not just by physical exertion [26], [27], but also by emotional stress [28], [29]. While we could gather additional insights by examining changes in heart rate variability (HRV) [28], [30], unfortunately, we were unable to assess this aspect in the current study.
– JT interval duration, measured in ms. In an electrocardiogram, this is the interval from junction point J to the end of the T wave. The duration of the JT interval describes the duration of ventricular repolarization. Changes in the JT interval are influenced by the regulatory nervous system. Metabolic changes in the body are known to be associated with changes in repolarization.
– QRS, measured in ms, is the duration of the QRS complex or excitation spread in the heart, which describes the internal regulatory system of the heart [31].
Fig. 1Cardiac intervals
2.4. Procedures
6ABT group received short- 6 days- outpatient BT complex course: Tap water pool with light exercises – 20 min, 34-36° mineral/geothermal water bath – 20 min, sapropel wrapping – 20 min, salt therapy – 25 min. 11ABT group received 11 days outpatient same BT complex. 11ABTNT group received 11 days outpatient BT complex plus natural therapy procedure developed by the researchers: a 45-minute walk in nature (forest, seaside), a complex of simple strength and breathing low-intensity exercises, sensory impulses (landscape, forest smells – aromatherapy, natural sounds of nature, collecting nature’s goodies, mindfulness therapy, heliotherapy. 11BTS group received 11 days inpatient treatment with the same BT complex. 11NT group received 11 days nature therapy procedure same as 11ABTNT group. 11C group was control group with no treatment.
The mineral water used in spa centers was 16.750-82.445 g/l total mineralization (dominant macroions were Cl, Na, Ca, Mg, SO4); peloids used were pH 6.6-7.0, humidity 70.5-96, total mineralization 38.5-20000 mg/l, dry residue 238-24.140 mg/l, botanical composition: reeds 60-80 %, sedges 10-30 %, organic material 14.32-91.96 %, degree of fragmentation 73-81.36 %, humic acid content 1.22-28.25, fulvic acid content 0.98-17.90 %.
2.5. Statistical analysis
Descriptive statistics were used to summarize the results of the questionnaire and determine the reduction of cardiovascular risk factors cardiovascular risk. Descriptive data are presented as means and SD (standard deviations) graphically by means and 95 % CI. Independent two-tailed t-tests were conducted for continuous variables, while a Chi-square test was utilized to compare variable frequencies across each rehabilitation group. Additionally, a z-test for categorical variables was employed to examine differences between categories. Analysis of variance (ANOVA) with Tukey HSD post-hoc multiple comparison tests were used to assess the differences between mean values of variables across the rehabilitation groups. Comparison of variable means at the beginning (T0), end (T1), three month (T2) and half a year (T3) of rehabilitation was performed using GLM Repeated Measures. GLM Repeated Measures analyzes groups of related dependent variables that represent different measurements of the same attribute. The Bonferroni test was used for statistically significant comparisons of mean differences. When the conditions of normality of the variables were not met, the differences between the values of the variables in the rehabilitation groups were evaluated by applying the Friedman non-parametric test. Interdependencies of quantitative variables were assessed using the Pearson correlation coefficient, and categorical variables – using the Spearman correlation coefficient. A p value < 0.05 denoted statistical significance.
Analyses were performed with the SPSS (Statistical Package for the Social Sciences for Windows). Version 28.0 SPSS Inc., Chicago, IL.
3. Results
The subjects’ sociodemographic and lifestyle-related issues are shown in Table 1. The average age of participants was 47.18 years, most were women, married, with high education, white-collar workers with average salary of 1000-1500-euro, work experience of > 20 years, almost half had working time up to 8, resting time – 7-8 hours, most were ill with Covid-19 and just 5-19 % apply healthy diet. There was no difference between the groups for these characteristics.
The significant reduction of systolic BP (–7.8 mm Hg, 5.7 %, p<0.05) after treatments and during 6-month follow up (up to 7.3 mm Hg, p<0.005) was achieved in 11 days ABT complex group and reached normal BP level [32] (Fig. 2). In all 11-day treatment groups (11 ABT, 11 ABTNT, 11 BTS, and 11 NT), a significant long-term reduction in systolic blood pressure up to 6 months was observed. There was no statistically significant difference between the study groups.
Although almost all therapeutic groups showed a positive change in diastolic blood pressure, a significant reduction was observed only after the 6-month period (up to 5.46 mm Hg, 6.4 %, p<0.05) in the 11-days BTS group, aiming to reach a normal level [32] (Fig. 3). Differences between groups were statistically significant after 3 months, with diastolic blood pressure (DBP) values differing significantly between 11BTS and 11NT groups (DBP in the 11NT group was 7.25 mm Hg lower than in the 11BTS group, p<0.05). After 6 months, the DBP value in the 11ABTNT group was 6.73 mm Hg lower than the control group (11C) (p<0.05).
The significant reduction in heart rate was observed in the 6-day group (4 beats/min, CI 0.172 – 8.228, p=0.037) and the 11-day ABT group (4 beats/min after treatment, CI 0.055-8.714, p=0.046) (Fig. 4).
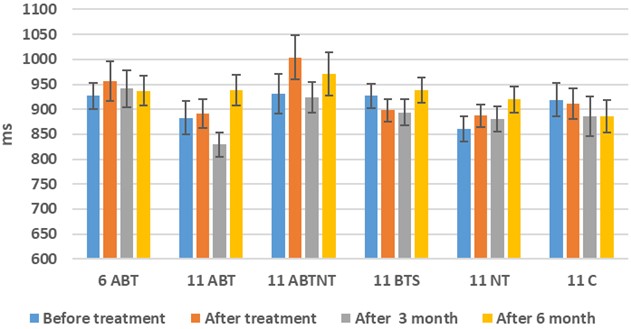
In the study, we analyzed the changes in the short-term ECG indicators RR, JT, and QRS immediately after the treatment course, at 3 months, and at 6 months post-treatment. Although there is no statistically significant difference in the RR indicator, an elongation in RR duration is observed after the treatment, most notably in the 11-day inpatient treatment group (Fig. 5).
Table 1The subjects’ characteristics in study groups
6ABT N = 18 | 11ABT N = 18 | 11ABTNT N = 15 | 11BTS N = 30 | 11NT N = 29 | 11C N= 21 | Pearson Chi-Square (2-sided) | |
Age, years ± SD | 44.72± 9.56 | 44.39± 13.9 | 47.33± 7.05 | 50.53 ±10.83 | 46.34 ±11.99 | 47.95± 11.86 | 0.431 |
BMI ± SD | 26.43± 6.38 | 26.12± 4.32 | 26.32± 4.11 | 27.44± 4.70 | 25.30± 5.13 | 27.18± 5.75 | 0.769 |
Gender, female (Male) | 11 (7) | 13 (5) | 13 (2) | 23 (7) | 25 (4) | 16 (5) | 0.41 |
Marital status, married, N (%) | 14 (77.8) | 11 (61.1) | 10 (66.7) | 15 (50.0) | 18 (62.1) | 16 (76.2) | 0.333 |
Education, University level, N (%) | 12 (66.7) | 10 (55.6) | 8 (53.3) | 19 (63.3) | 21 (72.4) | 13 (61.9) | 0.746 |
Profession, White-collar, N (%) | 10 (55.6) | 7 (38.9) | 7 (46.7) | 19 (63.3) | 18 (62.1) | 9 (42.86) | 0.216 |
Nature of work, Sedentary, N (%) | 8 (44.4) | 9 (50.0) | 5 (33.3) | 15 (50.0) | 15 (51.7) | 9 (42.86) | 0.970 |
Salary, 1000-1500 Euro, N (%) | 9 (50.0) | 9 (50.0) | 6 (40.0) | 11 (36.7) | 10 (34.5) | 10 (47.62) | 0.574 |
Work experience, > 20 years, N (%) | 13 (72.2) | 9 (50.0) | 11 (73.3) | 24 (80.0) | 19 (65.5) | 15 (71.43) | 0.173 |
Working time, ≤ 8 hours, N (%) | 9 (50.0) | 13 (72.2) | 5 (33.3) | 15 (50) | 17 (58.6) | 9 (29.0) | 0.536 |
Rest time, 7-8 hours, N (%) | 5 (27.8) | 9 (50.0) | 6 (40.0) | 10 (33.3) | 16 (55.2) | 8 (25.8) | 0.550 |
Covid-19 infection, N (%) | 15 (83.3) | 13 (72.2) | 14 (93.3) | 16 (53.3) | 22 (75.9) | 19 (61.3) | 0.295 |
Alcohol consumption, 2-3 times/week, N (%) | 5 (27,8) | 6 (33.3) | 4 (26.7) | 7 (23.3) | 10 (34.5) | 7 (22.6) | 0.365 |
Non-smoking N (%) | 14 (77.8) | 16 (88.9) | 13 (86.7) | 24 (80.0) | 25 (86.2) | 16 (51.6) | 0.675 |
Physical activity, 2-3 times/week, N (%) | 6 (33.3) | 6 (33.3) | 3 (20.0) | 7 (23.3) | 16 (55.2) | 7 (22.6) | 0.654 |
Ordinary diet, N (%) | 13 (72.2) | 13 (72.2) | 9 (60) | 21 (70.0) | 21 (72.4) | 12 (38.7) | 0.276 |
Fig. 2The change of systolic BP in study groups during 6-month observation period (*p< 0.05)
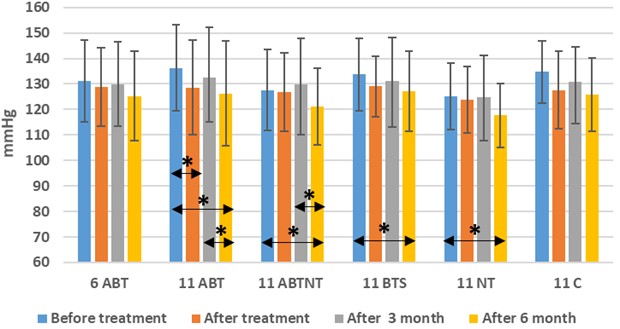
Fig. 3The change of diastolic BP in study groups during 6-month observation period (*p< 0.05)
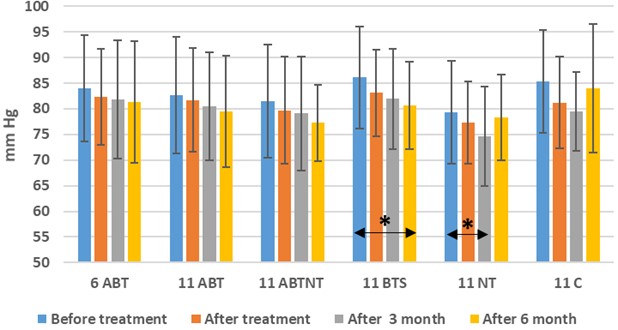
Fig. 4The change of HR in study groups during 6-month observation period (*p< 0.05)
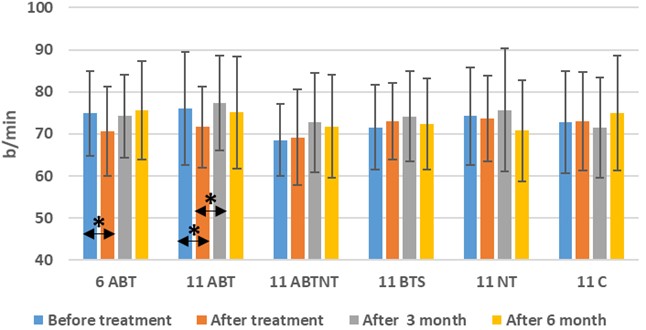
Fig. 5The change of ECG RR interval in study groups during 6-month observation period
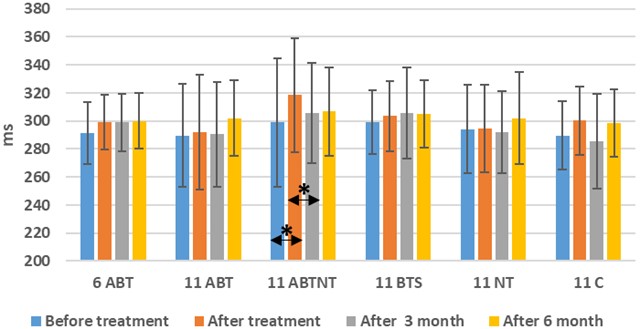
The JT interval reflects metabolic processes in the body. A statistically significant change in the JT interval was observed in the 11-day inpatient balneotherapy group. The JT interval extended by 19.71 ms (CI –35.346-(–4.082), p= 0.011). After 3 months, there was no significant difference in the measured duration of the JT interval compared to before the treatment course (Fig. 6).
Fig. 6The change of ECG JT interval in study groups during 6-month observation period (*p< 0.05)
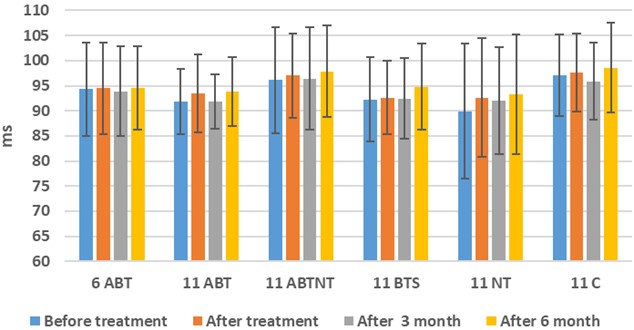
During the study, no statistically significant changes were observed in the QRS interval, although a somewhat more pronounced alteration in QRS duration was noted in the 11ABT and 11NT groups: the QRS complex duration increased by 1.647 ms in the 11ABT group and by 2.69 ms in the 11NT group (Fig. 7).
Fig. 7The change of ECG QRS interval in study groups during 6-month observation period
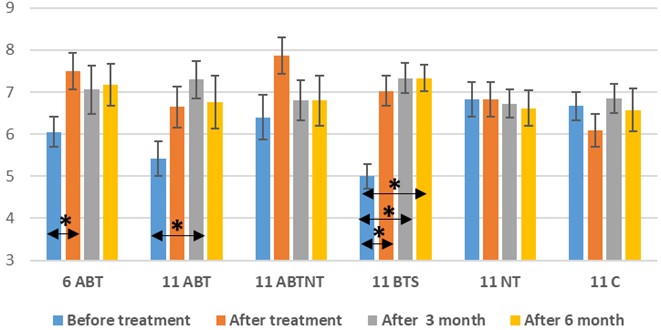
The stress intensity was significantly reduced after treatment and during the follow-up period in all four BT complex groups. The greatest mean difference (42.9 %) after treatment reached 2.434 (VAS, CI 1.43-3.44, p<0.001) in the 11-day inpatient group, and statistically significant differences persisted at 3 months after the balneotherapy course. In the NT group, the effect was short-term, returning to the initial level after 3 months (Fig. 8).
Stress management improved in the 6 ABT, 11 ABT, and 11 BTS complex groups. In the 6 ABT group, a significant short-term improvement in stress management was observed, but there was no significant difference after 3 months. In the 11 ABT group, improvement was observed immediately after treatment, but a significant enhancement was noted 3 months after the completed 11-day BT treatment in outpatient settings. The most significant long-term improvement was observed in the 11 BTS group. After treatment, a 40.66 % improvement (CI –2.876-(–0.013), p<0.001) was observed, persisting up to 6 months after treatment (Fig. 9).
Fig. 8The stress intensity in study groups (*p<0.05)
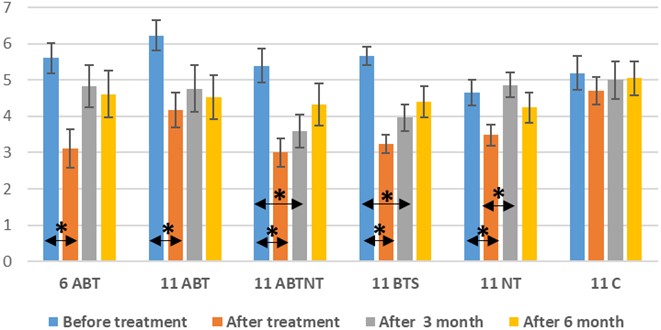
Fig. 9The stress management in study groups (*p<0.05)
4. Discussion
Natural resources are recognized among the key determinants for the improvement of wellness [33]. We discovered that treatment utilizing natural resources of Lithuania – such as mineral/geothermal water, peloids/therapeutic mud, and nature – results in a significant reduction of systolic and diastolic BP, HR, as well as a significant reduction in stress intensity, and an increase in stress management and parasympathetic activity. These positive changes of the important cardiovascular risk factors – BP, HR, stress, could be considered cautiously as a cardiovascular risk reduction also. The result of our BT complex treatment was reduction of systolic BP up to 7.8 mmHg. Meta-analysis showed that a 10 mm Hg reduction of systolic BP reduced the risk of major CVD events by 20 %, coronary heart disease by 17 %, stroke by 27 %, heart failure by 28 %, and death from all causes by 13 % [34]. According to [33], 20 minutes per day, 5 days per week, for a total 15 days BT cause the mean changes in pulse and systolic and diastolic BP of the group without hypertension 0.10±4.14 beats/min, 1.25±10.77 mm Hg, and 0.91±7.93 mm Hg, respectively. The study of Paran et al. [35] showed a significant reduction in systolic and diastolic BP. In another study where systolic and diastolic BR and HR were measured during treatment session it was concluded that BT may be effective for improving peripheral cardiopulmonary responses in patients with musculoskeletal disorders [21]. In another trial systolic BP measured before and after BT from day 1 to day 15 did not present a meaningful trend as well as diastolic BP in non-hypertensive and controlled groups, but HR was found as significantly different [36]. In similar study, bathing for 2×20 minutes in winter resulted in a decrease in BP (systolic by 10.0%; diastolic by 22.1%, p < 0.001), with both systolic and diastolic BP reduced by around 10 mmHg. The authors concluded that hot spring bathing could potentially improve cardiovascular function by reducing cardiac workload and inducing vasodilation effects [15]. The differences in results could be attributed to variations in the study population, comorbidities, duration of treatment, different treatment protocols and resources, as well as the timing of parameter measurements. The effect of BT on the cardiovascular system depends fundamentally on its hydrostatic pressure and heat effect. BT increases the hydrostatical pressure by means of significantly raising venous circulation [36]. We observed the reduction of HR up to 4 beat/min after BT. According to Ref. [7] each 10 beats per minute increase in the resting HR can substantially increase the risk of adverse CV and mortality outcomes; and reducing resting HR by at-least 10 bpm from baseline may provide benefits which need to be confirmed in prospective studies. The reaction of the human body to environmental influences is a complex reaction involving the functions of many systems. Changes in BP and HR are a characteristic response of the body to other factors affecting it. Nearly half of adults have hypertension (48.1 %, 119.9 million), or are taking medication for hypertension [37] so finding additional solution for BP management is worth it. According expert Opinion, HR has inverse relation with the central aortic pressure which affects CV outcomes in patients with hypertension [7]. Future studies are warranted to test implementation strategies for hypertension prevention and control [38]. All the parameters of ECG were within the normal range during study [39]. We investigated the changes of RR, JT and QRS intervals. A single ECG feature, such as the RR interval, which is a systemic parameter, indicates the functional status of the entire organism’s regulatory system and is used as a measure of neurocardiac function that reflects heart-brain interactions and ANS dynamics [40]. Predominant parasympathetic reflexes are indicated by a greater prolongation of the RR interval [41] as we also reveled in our study. JT is related to cardiac metabolic processes; QRS complex duration characterizes regulatory system processes related to cardiac intrinsic regulatory processes, conduction [31]. During spa resort treatment, the activity of the vegetative nervous system changes. In some cases, the general tension of the vegetative nervous system or only sympathetic activity decreases, in other cases, parasympathetic impulses are activated or their balance is restored [30]. As a result of the spa treatment, the opposite changes are visible: all duration ECG indicators (RR, JT and QRS) increased after the spa treatment, and the JT interval changes more intensively than the RR interval. This is especially evident in the inpatient treatment group, where the subjects had a full opportunity to relax. A significant increase in the duration of the JT interval (within the normal range) confirms the fact that treatment with spa factors in inpatient conditions is more effective (in terms of activation of the parasympathetic nervous system) compared to spa treatment when it is applied on an outpatient basis.
ECG metrics could be independent risk markers for cardiovascular death (hazard ratio, 95 % confidence interval): PR interval ≥ 200 ms (1.62, 1.19-2.19); QRS interval 100-119 ms (1.64, 1.20-2.25) and ≥ 120 ms (1.75, 1.17-2.62); corrected QT (QTc) interval ≥ 450 ms in men or ≥ 460 ms in women (1.72, 1.19-2.49); and heart rate 60-90 beats per minute (1.21, 0.89-1.63) and ≥ 90 beats per minute (2.35, 1.03-5.33) [42]. Identification of self-regulating system control mechanisms, complex dynamics in the human cardiovascular system, relationships between cardiac intervals in ECG could save lives [25], [27]. The effect on stress intensity and management was similar as in our previous works where 10-days geothermal water bath reduced stress intensity by 2.25 and increased management by 1.98 [43].
We found significant (2- tailed) correlation (Pearson) of systolic BP with diastolic BP (0.753, p<0.001), HR (0.232, p=0.008), and gender (0.20, p=0.022); diastolic BP- with systolic BP, HR (0.212, p=0.016), and gender (0.175, p=0.016); HR correlate with systolic and diastolic BP, work experience (–0.226, p=0.011). Stress intensity correlate with stress management (–0.298, p<0.001). It shows that by controlling one symptom, we are simultaneously improving another condition. No correlation with physical activity, smoking, alcohol consumption, work factors was not found. In appreciation of the fact that our BT complex used positively influenced the few health risk factors, it is beneficial for the individual, society and the economy to have an effective and safe multifunctional tool.
5. Strength and limitations of study
Our study contributes significantly to the limited body of research on balneotherapy for cardiovascular and mental health. We observed notable improvements in cardiovascular and psychological health parameters following treatment with natural resources found in Lithuania, including mineral/geothermal water, peloids, and exposure to nature. These positive changes suggest a potential reduction in cardiovascular risk. We conducted a parallel group study with different balneotherapy modalities and performed ECG parameters analysis, enhancing the depth of our findings. Moreover, such a study could contribute to the growing body of evidence supporting the integration of complementary and alternative medicine approaches into mainstream cardiovascular care.
Despite these strengths, our study faced certain limitations. A significant number of respondents were lost to follow-up, which may have introduced bias and affected the generalizability of our findings. Additionally, we were unable to draw clear conclusions about the optimal natural resource or treatment mode, as well as the specific mechanisms of action responsible for the observed effects. Looking forward, while balneotherapy shows promise for preventive medicine and health promotion, further research is warranted. Future studies should include a larger number of participants, ensure better compliance, and consider different groups with normal or elevated blood pressure, while also addressing other cardiovascular risk factors. Additionally, incorporating mathematical models to quantify the impact of balneotherapy on overall cardiovascular risk would strengthen future conclusions. High-quality, longer-term follow-up studies are needed to assess morbidity and mortality outcomes and evaluate the impact of interventions using natural factors on cardiovascular disease risk.
6. Conclusions
Our study underscores the potential of natural resources, particularly balneotherapy, as a promising adjunct to conventional approaches for cardiovascular risk reduction. We demonstrated that a 2-week balneotherapy intervention utilizing natural resources such as mineral water, peloid, salt procedures, and nature therapy effectively lowered blood pressure, heart rate, and stress levels while activating the parasympathetic nervous system. By offering a potentially effective and well-tolerated intervention, BT could broaden the options available for cardiovascular risk reduction and enhance the personalized management of patients with or at risk of cardiovascular conditions. Integrating such interventions into clinical practice has the potential to yield significant benefits in alleviating the burden of cardiovascular diseases.
References
-
F. Coronado, S. C. Melvin, R. A. Bell, and G. Zhao, “Global responses to prevent, manage, and control cardiovascular diseases,” Preventing Chronic Disease, Vol. 19, p. 22034, Dec. 2022, https://doi.org/10.5888/pcd19.220347
-
“Causes of death of Lithuanian residents in 2010-2022.” Health Statistics, https://www.hi.lt/php/dem13.php?dat_file=dem13.txt
-
“Confronting the world’s number one killer,” World Heart Federation, Geneva, Switzerland, 2023.
-
S. E. Kjeldsen, “Hypertension and cardiovascular risk: General aspects,” Pharmacological Research, Vol. 129, pp. 95–99, Mar. 2018, https://doi.org/10.1016/j.phrs.2017.11.003
-
“Hypertension,” World Health Organization, 2023.
-
G. Antonakoudis, L. Poulimenos, K. Kifnidis, C. Zouras, and Antonakoudis H., “Blood pressure control and cardiovascular risk reduction,” Hippokratia, Vol. 11, No. 3, pp. 114–119, 2007.
-
J. Dalal et al., “Heart rate in hypertension: review and expert opinion,” International Journal of Hypertension, Vol. 2019, pp. 1–6, Feb. 2019, https://doi.org/10.1155/2019/2087064
-
G. Mulè’, E. Nardi, M. Guarneri, and S. Cottone, “Electrocardiography for assessment of hypertensive heart disease: a new role for an old tool,” The Journal of Clinical Hypertension, Vol. 18, No. 9, pp. 843–845, May 2016, https://doi.org/10.1111/jch.12833
-
H. Nabi et al., “Increased risk of coronary heart disease among individuals reporting adverse impact of stress on their health: the Whitehall II prospective cohort study,” European Heart Journal, Vol. 34, No. 34, pp. 2697–2705, Sep. 2013, https://doi.org/10.1093/eurheartj/eht216
-
G. D. Batty, T. C. Russ, E. Stamatakis, and M. Kivimäki, “Psychological distress and risk of peripheral vascular disease, abdominal aortic aneurysm, and heart failure: pooling of sixteen cohort studies,” Atherosclerosis, Vol. 236, No. 2, pp. 385–388, Oct. 2014, https://doi.org/10.1016/j.atherosclerosis.2014.06.025
-
R. Gupta and S. Guptha, “Strategies for initial management of hypertension,” Indian Journal of medical research, Vol. 132, No. 5, pp. 531–542, 2010.
-
D. Matei et al., “Impact of non-pharmacological interventions on the mechanisms of atherosclerosis,” International Journal of Molecular Sciences, Vol. 23, No. 16, p. 9097, Aug. 2022, https://doi.org/10.3390/ijms23169097
-
L. D. Kubzansky et al., “Positive psychological well-being and cardiovascular disease,” Journal of the American College of Cardiology, Vol. 72, No. 12, pp. 1382–1396, Sep. 2018, https://doi.org/10.1016/j.jacc.2018.07.042
-
D. Shanahan et al., “Nature-based interventions for improving health and wellbeing: the purpose, the people and the outcomes,” Sports, Vol. 7, No. 6, p. 141, Jun. 2019, https://doi.org/10.3390/sports7060141
-
P.-C. Wang, Q.-C. Song, C.-Y. Chen, and T.-C. Su, “Cardiovascular physiological effects of balneotherapy: focused on seasonal differences,” Hypertension Research, Vol. 46, No. 7, pp. 1650–1661, Mar. 2023, https://doi.org/10.1038/s41440-023-01248-4
-
D. Yuan, Z.-X. Yu, W. Wang, and Y. Chen, “Head-out immersion in natural thermal mineral water for the management of hypertension: a review of randomized controlled trials,” International Journal of Biometeorology, Vol. 63, No. 12, pp. 1707–1718, Aug. 2019, https://doi.org/10.1007/s00484-019-01780-4
-
T. Kataoka et al., “Association between radon hot spring bathing and health conditions: a cross-sectional study in Misasa, Japan,” Acta Medica Okayama, Vol. 77, No. 4, pp. 387–394, Aug. 2023, https://doi.org/10.18926/amo/65749
-
C. Ekmekcioglu, G. Strauss-Blasche, J. Feyertag, N. Klammer, and W. Marktl, “The effect of balneotherapy on ambulatory blood pressure,” Alternative therapies in health and medicine, Vol. 6, No. 6, pp. 46–53, Nov. 2000.
-
S. V. Klemenkov, O. B. Davydova, E. F. Levitskiĭ, N. F. Chashchin, O. Ia Sharova, and I. V. Kubushko, “The effect of sodium chloride baths on the physical work capacity and extrasystole of patients with ischemic heart disease and stable stenocardia,” Voprosy Kurortologii, Fizioterapii, I Lechebnoi Fizicheskoi Kultury, Vol. 3, No. 3, pp. 19–21, 1999.
-
J. L. Cheng and M. J. Macdonald, “Effect of heat stress on vascular outcomes in humans,” Journal of Applied Physiology, Vol. 126, No. 3, pp. 771–781, Mar. 2019, https://doi.org/10.1152/japplphysiol.00682.2018
-
S. Şaş, Toprak Çelenay, and D. Özer Kaya, “The effects of balneotherapy on acute, process-related, and cumulative peripheral cardiac responses and pulmonary functions in patients with musculoskeletal disorders,” Turkish Journal of Medical Sciences, Vol. 46, No. 6, pp. 1700–1706, Jan. 2016, https://doi.org/10.3906/sag-1505-31
-
S. Cheleschi, I. Gallo, and S. Tenti, “A comprehensive analysis to understand the mechanism of action of balneotherapy: why, how, and where they can be used? Evidence from in vitro studies performed on human and animal samples,” International Journal of Biometeorology, Vol. 64, No. 7, pp. 1247–1261, Mar. 2020, https://doi.org/10.1007/s00484-020-01890-4
-
I. Gálvez, S. Torres-Piles, and E. Ortega-Rincón, “Balneotherapy, immune system, and stress response: a hormetic strategy?,” International Journal of Molecular Sciences, Vol. 19, No. 6, p. 1687, Jun. 2018, https://doi.org/10.3390/ijms19061687
-
S. Cheleschi, S. Tenti, I. Seccafico, I. Gálvez, A. Fioravanti, and E. Ortega, “Balneotherapy year in review 2021: focus on the mechanisms of action of balneotherapy in rheumatic diseases,” Environmental Science and Pollution Research, Vol. 29, No. 6, pp. 8054–8073, Nov. 2021, https://doi.org/10.1007/s11356-021-17780-0
-
Ragulskis M., “Algebraic relationships between cardiac intervals for deeper insight into the self-organization of the human cardiovascular system,” in Workshop on Computer Methods in Medicine and Health Care (CMMHC 2023), 2023.
-
A. Vainoras, D. Ašeriškytė, J. Poderys, and Z. Navickas, “Fractal dimensions in evaluation of heart function parameters during physical investigations,” Baltic Journal of Sport and Health Sciences, Vol. 3, No. 57, pp. 61–66, Nov. 2018, https://doi.org/10.33607/bjshs.v3i57.641
-
N. W. Qammar, U. Orinaitė, V. Šiaučiūnaitė, A. Vainoras, G. Šakalytė, and M. Ragulskis, “The complexity of the arterial blood pressure regulation during the stress test,” Diagnostics, Vol. 12, No. 5, p. 1256, May 2022, https://doi.org/10.3390/diagnostics12051256
-
Mccraty Rollin, Atkinson Mike, Tomasino Dana, and Raymond Trevor Bradley, “The coherent heart heart-brain interactions, psychophysiological coherence, and the emergence of system-wide order,” Integral Review, Vol. 5, No. 2, Dec. 2009.
-
J. Elbers and R. Mccraty, “HeartMath approach to self-regulation and psychosocial well-being,” Journal of Psychology in Africa, Vol. 30, No. 1, pp. 69–79, Feb. 2020, https://doi.org/10.1080/14330237.2020.1712797
-
G. Taletavičienė, K. Ramanauskas, G. Jaruševičius, and A. Vainoras, “Heart rhythm fluctuation in peloidotherapy,” Journal of Vibroengineering, Vol. 15, No. 1, pp. 428–437, Mar. 2013.
-
G. Taletaviciene, “Changes of electrocardiographic parameters and their dynamic concatenations during whole-body cryotherapy and peloidotherapy procedures,” Kaunas: LSMU, 2014.
-
J. M. Flack and B. Adekola, “Blood pressure and the new ACC/AHA hypertension guidelines,” Trends in Cardiovascular Medicine, Vol. 30, No. 3, pp. 160–164, Apr. 2020, https://doi.org/10.1016/j.tcm.2019.05.003
-
E. Pessot, D. Spoladore, A. Zangiacomi, and M. Sacco, “Natural resources in health tourism: a systematic literature review,” Sustainability, Vol. 13, No. 5, p. 2661, Mar. 2021, https://doi.org/10.3390/su13052661
-
D. Ettehad et al., “Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis,” The Lancet, Vol. 387, No. 10022, pp. 957–967, Mar. 2016, https://doi.org/10.1016/s0140-6736(15)01225-8
-
E. Paran, L. Neuman, and S. Sukenik, “Blood pressure changes at the Dead Sea (a low altitude area),” Journal of Human Hypertension, Vol. 12, No. 8, pp. 551–555, Aug. 1998, https://doi.org/10.1038/sj.jhh.1000663
-
E. Hayta, M. Yilmaz, I. Yayikçi, Z. Özer, and Sahin, “Is there a clinically meaningful change in the blood pressure of osteoarthritis patients with comorbid hypertension during the course of balneotherapy?,” North American Journal of Medical Sciences, Vol. 7, No. 11, p. 517, Jan. 2015, https://doi.org/10.4103/1947-2714.170616
-
“Hypertension cascade: hypertension prevalence, treatment and control estimates US adults aged 18 years and older applying the criteria from the American College of Cardiology and American Heart Association’s 2017,” US Department of Health and Human Services, 2021.
-
K. T. Mills, A. Stefanescu, and J. He, “The global epidemiology of hypertension,” Nature Reviews Nephrology, Vol. 16, No. 4, pp. 223–237, Feb. 2020, https://doi.org/10.1038/s41581-019-0244-2
-
L. Rosenthal, “Normal Electrocardiography (ECG) Intervals,” Medscape, 2020.
-
F. Shaffer, R. Mccraty, and C. L. Zerr, “A healthy heart is not a metronome: an integrative review of the heart’s anatomy and heart rate variability,” Frontiers in Psychology, Vol. 5, pp. 1–19, Sep. 2014, https://doi.org/10.3389/fpsyg.2014.01040
-
R. Ablonskytė-Dūdonienė and E. Ereminienė, “Autonomic heart rate regulation and its changes in myocardial infarction and diabetes mellitus,” Medicine (Kaunas), Vol. 46, No. 3, pp. 219–230, 2010.
-
R. Deo et al., “Electrocardiographic Measures and Prediction of Cardiovascular and Noncardiovascular Death in CKD,” Journal of the American Society of Nephrology, Vol. 27, No. 2, pp. 559–569, Feb. 2016, https://doi.org/10.1681/asn.2014101045
-
L. Rapolienė, A. Razbadauskas, J. Sąlyga, and A. Martinkėnas, “Stress and fatigue management using balneotherapy in a short-time randomized controlled trial,” Evidence-Based Complementary and Alternative Medicine, Vol. 2016, pp. 1–10, Jan. 2016, https://doi.org/10.1155/2016/9631684
About this article
We express our gratitude to all the researchers involved in the LUGISES project, as well as to the chief executives of the research centers Gradiali, Eglė, Draugystė, Tulpė, Versmė, and Atostogų parkas for their administrative and technical support. Additionally, we appreciate the dedication and assistance of the staff at the research centers and Klaipeda University in conducting the clinical research. This research was funded by Research Council of Lithuania, grant number S-REP-22-6. Project “Effectiveness and safety of the use of Lithuania’s unique natural resources for improving the mental and physical health of the organism experiencing stress” (LUGISES).
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Lolita Rapolienė: conceptualization, data curation, formal analysis, investigation, methodology, project administration, validation, visualization, writing-original draft preparation, writing-review and editing. Giedrė Taletavičienė: conceptualization, formal analysis, resources, software, supervision, writing-original draft preparation. Arvydas Martinkėnas: conceptualization, data curation, formal analysis, validation.
The authors declare that they have no conflict of interest.
The study was conducted in accordance with the Declaration of Helsinki. The research met all applicable standards for the ethics of experimentation. Participants provided written informed consent prior to the experiment. Permit to perform biomedical investigation was granted by Kaunas Regional Research Ethics Committee (resolution No BE-2-87). The trial was registered in ClinicalTrial.gov (Identifier: NCT06018649).

