Abstract
Over the past few years, the early mobilization and rehabilitation of patients in the intensive care unit (ICU) has drawn a lot of interest from the clinical and scientific communities. An interdisciplinary team treating patients suffering from serious conditions should include physiotherapy. Additionally, physiotherapy is utilized to treat and prevent the side effects of extended immobility or sleep, as well as to improve respiratory function. The purpose is to improve residual functionality; to avoid new and repeated hospitalizations; to improve health and quality of life. Exercises for the entire body (including early in-bed cycling), specialized breathing exercises, chest mobilization, relief help, drainage postures, vibration, verticalization, and passive movements are all crucial components of COVID-19 physiotherapy. Our goal was to evaluate the changes of functional condition of patients with COVID-19 in the acute stage using different physiotherapy methods: complex measures against mono therapy. In the research, 28 subjects (15 men and 13 women) were involved. A total of 84 physiotherapy procedures were performed. In the first group, breathing exercises and chest wall oscillation were applied, in the second group – only chest wall oscillation. Respiratory physiotherapy (breathing exercises) plays an important role in reducing and preventing respiratory complications in COVID-19 patients treated at ICU. Early mobilization and chest wall oscillation are beneficial in COVID-19 patients. We note that we are the first to conduct an evidence-based study of physiotherapy in intensive care with COVID-19 patients. We hope that our pilot clinical trial gives opportunity to future researches.
Highlights
- Respiratory physiotherapy (breathing exercises) plays an important role in reducing and preventing respiratory complications in COVID-19 patients treated at ICU.
- Early mobilization and chest wall oscillation are beneficial in COVID-19 patients.
- Complex using different physiotherapy methods are better than mono therapy if we need changes of functional condition of patients with COVID-19 in the acute stage.
1. Introduction
On December 31, 2019, the infection caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was originally reported as Coronavirus disease (COVID-19) [1]. The global impact of the Coronavirus 2019 (COVID-19) pandemic has been unprecedented, with intensive care unit (ICU) care and ventilator availability at the center of health resource allocation and planning [2]. Fever (98 percent), cough (76 percent), and myalgia or weariness (44 percent) are the most common signs and symptoms of the disease; other symptoms include sputum, headache, hemoptysis, vomiting, diarrhea, and dyspnea. Furthermore, many patients developed pneumonia, with acute respiratory distress syndrome being one of the most common consequences [3]. During the decurarization phase, patients begin acute rehabilitation. Patients may require oxygen therapy, non-invasive ventilation, including continuous positive airway pressure, intubation and admission to the ICU depending on the severity of their disease. Body temperature, respiratory rate, and oxygen saturation appear to be the most important clinical indicators. The length of stay in ICU has been reported to be greater than typical, with an average of three weeks [4].
Physical therapists are important in the fight against the COVID-19 pandemic because they help with the prevention and rehabilitation of COVID-19-related impairments, as well as assisting with functional independence and reintegration into society [5]. Dysphagia, muscle weakness, critical illness myopathy and neuropathy, reduced joint mobility, neck and shoulder pain (due to prolonged pronation), difficulty in verticalization, impaired balance and gait, limitations in activities of daily living, difficult awakening with long-term confusional state, and psychological problems have all been diagnosed so far. Some patients develop significant respiratory insufficiency due to lung fibrosis as a sequel of pneumonia, demanding respiratory rehabilitation or even non-invasive ventilation. Other patients create thick secretions that necessitate physiotherapy or technical clearance [4].
The mucociliary escalator and the cough reflex are critical mechanisms in maintaining a healthy and functional respiratory system: they avoid obstruction and provide enough airflow through the lungs by clearing secretions that could otherwise accumulate in the airways [6]. For acute pneumonic patients receiving endotracheal intubation, mechanical ventilation, and sedation, coughing is not an option. As a result, these patients may have a lot of pulmonary secretions, which can lead to bronchial hygiene problems, low oxyhemoglobin saturation, poor ventilation-perfusion match, and lung atelectasis or collapse. High-frequency chest wall oscillation can remove airway secretions by simulating a “mini-cough” by compressing and relaxing the chest wall to generate an oscillated volume from the lungs [7]. Various ventilatory methods, such as early chest physiotherapy (CPT) and rehabilitation, may be required for different patients. In general, CPT maneuvers are regarded critical in patient management during an ICU stay [5]. Cardiorespiratory physiotherapy focuses on the treatment of acute and chronic respiratory disorders, with the goal of improving physical rehabilitation after a hospital stay. Patients with COVID-19 may benefit from physiotherapy for respiratory treatment and physical rehabilitation [6]. Early exercise and mobilization, the use of prone positions in the ICU are all elements that physical therapists work with in the treatment of COVID-19 patients [8].
Our goal was to evaluate the changes of functional condition of patients with COVID-19 in the acute stage using different physiotherapy methods: complex measures against mono therapy. In the research, 28 subjects (15 men and 13 women) were involved. A total of 84 physiotherapy procedures were performed. Physiotherapy was performed once a day for every patient. In the first group, breathing exercises and chest wall oscillation were applied, in the second group – only chest wall oscillation. Breathing exercises that we chose were diaphragmatic, mixed breathing, inhalations and exhalations combined with active movements of the limbs and torso performed by the patient himself. Chest wall oscillation is a secretion-reducing technique performed with the help of a high-intensity (16 Hz) vest.
2. Methods
2.1. Participants
The study included patients that were hospitalized with COVID-19 in the ICU. Twenty-eight COVID-19 patients (15 men and 13 women) were enrolled in the study. They were hospitalized in the ICU at Hospital of Lithuanian University of Health Sciences Kaunas Clinics. A total of 84 physiotherapy procedures were performed. There were no statistical differences between subjects of both groups. Demographic statistics are listed in Table 1.
Table 1Demographic statistics
First group (chest wall oscillation and exercises) | Second group (chest wall oscillation) | P value | |
Age | 57.5 (44-81; 58.36) years old | 51 (33-65; 51) years old | p>0,05 |
Gender | Men 8 (53.4 %) | Men 7 (46.6 %) | |
Women 6 (46.2 %) | Women 7 (53.8 %) | ||
FiO2 baseline | 85 (60-100; 84.29) | 86 (60-80; 85.14) | p>0,05 |
Inclusion criteria: the diagnosis of COVID-19 was confirmed by PCR and bilateral pneumonia was confirmed by radiological examination.
Exclusion criteria referred to patients who had a recent episode of myocardial ischemia, had severe neurological diseases, HR < 40 or >130 BPM, mean arterial blood pressure < 60 mmHg and > 110 mmHg, body temperature ≥ 38.5 °C and ≤ 36 °C, The Richmond Agitation and Sedation Scale (RASS) –4, –5, 3, 4.
3. Outcome measures
Before and after each procedure, the following were recorded: 1) ventilation parameters: FiO2 – fraction of Inspired Oxygen (%), flow of oxygen (l/min); 2) heart rate (BPM); 3) arterial blood pressure (mmHg); 4) saturation – a clinical measure of the amount of oxygen in a patient’s blood (%); 5) cough nature and productivity (dry cough or cough with secretion).
3.1. Ventilation parameters
Physicians and nurses in intensive hospital care units monitor breathing parameters to analyze patients’ physical status. The needed oxygen concentration varies depending on the patient. Ventilation parameters such as FiO2 and oxygen flow were measured in this study. To maintain O2 saturation, FiO2 should be regulated. The high-flow nasal cannula is an oxygen therapy device that uses a specific nasal cannula to deliver properly heated and humidified oxygen at a rate of up to 60 L/min. The amount of oxygen in the gas mixture is measured by the percentage of inspired oxygen (FiO2). Varied FiO2 can be delivered via oxygen delivery tools like a nasal cannula, venturi mask, and high flow nasal cannula. A patient breathing room air is taking in air with a FiO2 of 21 %. Oxygen delivery devices use anticipated equipment algorithms to calculate the flow rate and FiO2 [10].
3.2. Heart rate and arterial blood pressure
The heart rate measures the number of times the heart beats per minute. Arterial blood pressure is defined as the force that is exerted by the blood on the arterial wall. The management of patients is heavily influenced by arterial blood pressure, a key cardiovascular variable that is regularly evaluated in perioperative and intensive care medicine [11].
3.3. Saturation (SpO2)
Peripheral capillary oxygen saturation is an essential element of patient care. Oxygen is tightly regulated within the body because hypoxemia can lead to many acute adverse effects on individual organ systems. Oxygen saturation is a measure of how much hemoglobin is currently bound to oxygen compared to how much hemoglobin remains unbound [9].
3.4. Cough nature and productivity
Coughs are frequently described as “wet”, “moist”, or “dry”. A moist cough is most likely caused by suppurative lung illness, while a loose, rattling cough is thought to be caused by excess secretions or exudates in the wider airways [12]. In this study cough was identified as dry (not productive) and cough with secretion (productive). The same specialist made a subjective assessment of cough.
4. Data analysis
Statistical analysis was performed using the “IBM SPSS Statistics 21” software package. The nonparametric Man – Whitney Wilcoxon criteria (U) was applied to the two independent samples. The nonparametric Wilcoxon criteria (Z) was applied for the two dependent samples. Quantitative data of tests results are described by median (Xme), minimum value (Xmin), maximum value (Xmax) and arithmetic mean (m) – Xme (Xmin-Xmax; m). The difference was considered statistically significant when was p<0.05. Qualitative data are described by percent (%).
5. Results
5.1. Fraction of inspired oxygen
In the chest wall oscillation + exercises group fraction of inspired oxygen before the intervention was 86 (60-80; 85.14) percent. After intervention it changed to 60 (0-100; 51.36) percent. This change was statistically significant (Z = –2.413; p=0.016).
In the chest wall oscillation group fraction of inspired oxygen before the intervention was 85 (60-100; 84.29) percent. After intervention fraction of inspired oxygen was 87.5 (0-100; 80.36) percent. This change was not statistically significant (Z = –0.239; p=0.811).
After comparing results of both groups before the intervention there was found no statistically significant difference (U = 92.5; p=0.81), but after the intervention significant difference was found (U = 56.5; p=0.038).
5.2. Flow of oxygen
In the first group, where chest wall oscillation and exercises were performed, flow of oxygen before the intervention was 50 (0-80; 48.93) l/mol. After the intervention in this group flow of oxygen changed to 32.5 (0-95; 30.86) l/mol. This change was statistically significant (Z = –1.958; p=0.048).
In the second group, where only chest wall oscillation was performed, flow of oxygen before the intervention was 67.5 (0-80; 57.14) l/mol. After the intervention in this group flow of oxygen switched to 50 (0-80; 43.21) l/mol. this change was statistically significant (Z = –2.615; p=0.009).
After comparing flow of oxygen results between groups there was no statistically significant changes found neither before (U = 68.5; p=0.178), nor after the intervention (U = 73.5; p=0.261).
5.3. Haemodynamic
In the first group (chest wall oscillation + exercises) hearth rate before the intervention was 79 (60-120; 82.29) bpm. After the intervention hearth rate was 83 (58-135; 86) bpm. There was found no significant difference between these data (Z = –0.691; p=0.49).
In the second group (only chest wall oscillation) heart rate before the intervention was 80 (53-124; 80.79) bpm. After the intervention in the same group hearth rate was 83 (46-117; 85.57) bpm. There was found no significant difference between these data in this group before and after the intervention (Z = –0.722; p=0.47).
After comparing hearth rate results between the groups neither before (U = 93.5; p=0.848) nor after the intervention (U = 93; p=0.83) there was found no significant difference.
After comparing systolic blood pressure results between groups there was no significant difference neither before (U = 73; p=0.26), nor after the intervention (U = 69; p=0.189).
After measuring diastolic blood pressure results of both groups between each other there was no statistically significant difference found neither before the intervention (U = 74.5; p=0.29), nor after (U = 83.5; p=0.517).
5.4. Saturation
In the group, where chest wall oscillation and exercises were performed, saturation before the intervention was 92.5 (88-98; 92.64) percent. After the intervention result was 94.5 (92-100; 95.07) percent. There was found significant difference between these results (Z = –1.966; p=0.049).
Table 2Results
n | Mean baseline | Mean change from baseline | Z-value p-value | Between groups before intervention | Between groups after intervention | |
Fraction of inspired oxygen chest wall oscillation + exercises group chest wall oscillation | 14 | 85.14 % | 51.36 % | Z = –2.413; p=0.016 | U = 92.5; p=0.81 | U = 56.5; p=0.038 |
14 | 84.29 % | 80.36 % | Z = –0.239; p=0.811 | |||
Flow of oxygen chest wall oscillation + exercises group chest wall oscillation | 14 | 48.93 l/mol | 30.86 l/mol | Z = –1.958; p=0.048 | U = 68.5; p=0.178 | U = 73.5; p=0.261 |
14 | 57.14 l/mol | 43.21 l/mol | Z = –2.615; p=0.009 | |||
Hearth rate chest wall oscillation + exercises group chest wall oscillation | 14 | 82.29 bpm | 86 bpm | Z = –0.691; p=0.49 | U = 93.5; p=0.848 | U = 93; p=0.83 |
14 | 80.79 bpm | 85.57 bpm | Z = –0.722; p=0.47 | |||
Systolic blood pressure chest wall oscillation + exercises group chest wall oscillation | 14 | 124.71 mm/Hg | 123.43 mm/Hg | Z = –0.283; p=0.777 | U = 73; p=0.26 | U = 69; p=0.189 |
14 | 118.43 mm/Hg | 115.64 mm/Hg | Z = –0.56; p=0.576 | |||
Diastolic blood pressure chest wall oscillation + exercises group chest wall oscillation | 14 | 68.64 mm/Hg | 67.86 mm/Hg | Z = –0.251; p=0.801 | U = 74.5; p=0.29 | U = 83.5; p=0.517 |
14 | 63.86 mm/Hg | 65.79 mm/Hg | Z = –0.472 p=0.637 | |||
Saturation chest wall oscillation + exercises group chest wall oscillation | 14 | 92.64 % | 95.07 % | Z = –1.966; p=0.049 | U = 79; p=0.391 | U = 91; p=0.755 |
14 | 91.29 % | 94.36 % | Z = –2.85; p=0.004 |
In the group, where only chest wall oscillation was performed, saturation before the intervention was 91 (83-97; 91.29) percent. After the intervention result was 95 (90-98; 94.36). There was found significant difference between these results (Z = –2.85; p=0.004).
After comparing saturation results before the intervention there was found no significant difference between the groups (U = 79; p=0.391). After the intervention there was also no significant difference found between the groups (U = 91; p=0.755).
The results are presented in Table 2.
5.5. Coughing
In the first group, where chest wall oscillation and exercises were performed, before the intervention 21.43 percent of subjects had no coughing, 35.71 percent of subjects had coughing with secretions and 42.86 percent of subjects had dry coughing. After the intervention 57.14 percent of subjects had no coughing, 21.43 percent of subjects had dry coughing and 21.43 percent of subjects had coughing with secretions. See at Fig. 1.
Fig. 11st group before a) and after b) the intervention
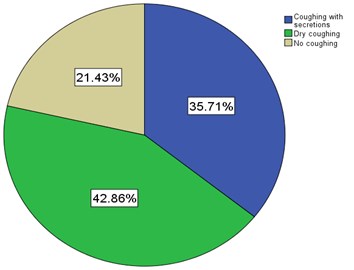
a)
b)
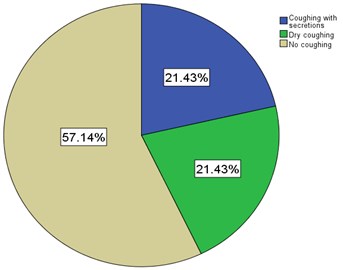
In the second group, where only chest wall oscillation were performed, before the intervention 50 percent of subjects had no coughing, 35.71 percent of subjects had coughing with secretions and 14.29 percent of subjects had dry coughing. After the intervention 57.14 percent of subjects had no coughing, 7.14 percent of subjects had coughing with secretions and 35.71 percent of subjects had dry coughing. See at Fig. 2.
Fig. 22nd group before a) and after b) the intervention
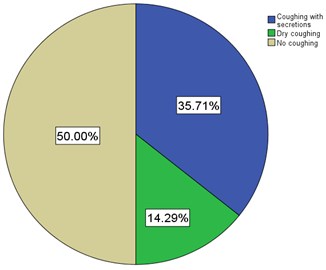
a)
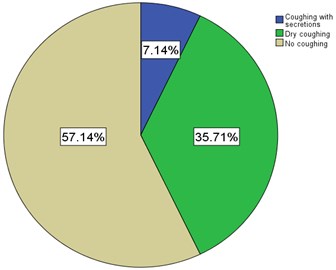
b)
5.6. Correlations
Correlation when |r|≤0,3 was accepted as very weak, 0,3 <|r|≤ 0,7 was accepted as moderate strong and |r|>0,7 was accepted as very strong.
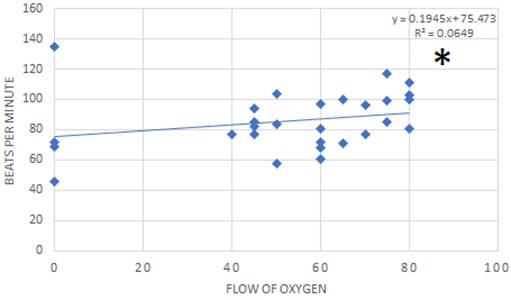
There was moderate strong correlation found between flow of oxygen and beats per minute. See at Fig. 3.
Fig. 3Statistically significant moderate strong correlation between results of flow of oxygen and beats per minute (r= 0.484; p= 0.009)
6. Discussions
Based on the studies by L. M. S. Dias et. al. (2022) and Aslıhan Çakmak et. al. (2019) the most frequently used respiratory techniques in the ICU were positioning (86 %), alveolar recruitment (73 %), and hard/brief expiratory rib cage compression (46 %), whereas those in the ward were active prone positioning (90 %), breathing exercises (88 %), and directed/assisted cough (75 %) [13], [14]. In our pilot clinical trial, mostly used physiotherapy methods were breathing exercises and chest wall oscillation.
N. Ambrosino et. al. (2011) claims that recovery of physical and respiratory functions, coming off mechanical ventilation, prevention of the effects of bed-rest and improvement in the health status are the clinical objectives of a physiotherapy program in medical and surgical areas. To manage these patients, integrated programs dealing with both whole-body physical therapy and pulmonary care are needed [15]. We observed that the amount of oxygen in the gas mixtured of inspired oxygen, flow of oxygen and oxygenation decrease suggests that the patient is recovering. This indicates that he needs less additional help with breathing.
Based on the results of the study by S. A. R. Younes et. al. (2022), it can be said that twice-daily multimodality chest physiotherapy interventions, such as manual hyperinflation, endotracheal suctioning, patient positioning, chest percussion, and mechanical chest vibration device, had a better impact on reducing the incidence of ventilator associated pneumonia and improving patient's clinical outcome [16]. Results of our study showed: in the group that applied breathing exercises and chest wall oscillation, the amount of oxygen in the gas mixtured of inspired oxygen and flow of oxygen decreased but saturation increased. In the group, where chest wall oscillation was applied, flow of oxygen decreased and saturation increased. The numbers in those who coughed with secretions decreased, dry cough increased, and the number of those who did not cough increased.
The World Association of Vibration Exercise Experts reviewed that whole body vibration exercise is a non-invasive physical therapy, which has been suggested as part of the procedures involved with pulmonary rehabilitation, even in ICU settings [17]. In our study, changes are observed in both groups, greater in the group in which chest wall oscillation was combined with breathing exercises. In this study cough was identified as dry (not productive) and cough with secretion (productive). At the beginning of treatment, when patients do not cough at all, the result is bad, because proper ventilation does not take place. It is very good when the cough becomes wet during the treatment. After treatment, the cough may disappear completely. Changes are observed in both groups.
It is evident that hospitalized COVID-19 patients require standardized respiratory physiotherapy care. Our study was limited by the absence of a third group with breathing exercises. Although methodologies are similar across countries and hospitals, there is a lack of generally accepted physiotherapy protocols for ICU patients in critical conditions. We note that we are the first to conduct an evidence-based study of physiotherapy in intensive care with COVID-19 patients. In our research, we proved that complex measures are better than mono therapy, which is the strength of this study. We hope that our pilot clinical trial gives opportunity to future researches. It is expected that the results and prepared clinical conclusions of this study will be useful for all specialists in the field of rehabilitation and reanimatologists working with respiratory diseases, as well as people with COVID-19 at various stages of their counseling or treatment.
7. Conclusions
Respiratory physiotherapy (breathing exercises) plays an important role in reducing and preventing respiratory complications in COVID-19 patients treated at ICU. Outcome measures changes were observed in both groups, greater in the group in which chest wall oscillation was combined with breathing exercises. Early mobilization and chest wall oscillation are beneficial in COVID-19 patients. There was moderate strong correlation found between flow of oxygen and beats per minute.
References
-
L. M. Sheehy, “Considerations for postacute rehabilitation for survivors of COVID-19,” JMIR Public Health and Surveillance, Vol. 6, No. 2, p. e19462, May 2020, https://doi.org/10.2196/19462
-
R. Chang, K. M. Elhusseiny, Y.-C. Yeh, and W.-Z. Sun, “COVID-19 ICU and mechanical ventilation patient characteristics and outcomes—A systematic review and meta-analysis,” PLOS ONE, Vol. 16, No. 2, p. e0246318, Feb. 2021, https://doi.org/10.1371/journal.pone.0246318
-
C. Bernal-Utrera, E. Anarte-Lazo, J. J. Gonzalez-Gerez, E. De-La-Barrera-Aranda, M. Saavedra-Hernandez, and C. Rodriguez-Blanco, “Could physical therapy interventions be adopted in the management of critically Ill patients with COVID-19? A scoping review,” International Journal of Environmental Research and Public Health, Vol. 18, No. 4, p. 1627, Feb. 2021, https://doi.org/10.3390/ijerph18041627
-
D. Y. Melesse and W. B. Chekol, “The management of patients with coronavirus disease 2019 in intensive care unit (ICU) in low income countries: A review article,” Clinical Nutrition Open Science, Vol. 37, pp. 60–72, Jun. 2021, https://doi.org/10.1016/j.nutos.2021.05.001
-
L. E. S. Paz, B. J. D. S. Bezerra, T. M. M. Pereira, and W. E. D. Silva, “COVID-19: the importance of physical therapy in the recovery of workers’ health,” Revista Brasileira de Medicina do Trabalho, Vol. 19, No. 1, pp. 94–106, 2021, https://doi.org/10.47626/1679-4435-2021-709
-
G. Leemans et al., “The effectiveness of a mobile high‐frequency chest wall oscillation (HFCWO) device for airway clearance,” Pediatric Pulmonology, Vol. 55, No. 8, pp. 1984–1992, Aug. 2020, https://doi.org/10.1002/ppul.24784
-
M.-L. Chuang, Y.-L. Chou, C.-Y. Lee, and S.-F. Huang, “Instantaneous responses to high-frequency chest wall oscillation in patients with acute pneumonic respiratory failure receiving mechanical ventilation,” Medicine, Vol. 96, No. 9, p. e5912, Mar. 2017, https://doi.org/10.1097/md.0000000000005912
-
S. Eggmann et al., “Early physical therapist interventions for patients with COVID-19 in the acute care hospital: a case report series,” Physical Therapy, Vol. 101, No. 1, Jan. 2021, https://doi.org/10.1093/ptj/pzaa194
-
A. M. Esquinas et al., Noninvasive Ventilation in Sleep Medicine and Pulmonary Critical Care. Cham: Springer International Publishing, 2020, https://doi.org/10.1007/978-3-030-42998-0
-
Fuentes S. and Chowdhury Ys, Fraction of Inspired Oxygen. StatPearls Publishing, 2022.
-
B. Saugel, K. Kouz, A. S. Meidert, L. Schulte-Uentrop, and S. Romagnoli, “How to measure blood pressure using an arterial catheter: a systematic 5-step approach,” Critical Care, Vol. 24, No. 1, pp. 1–10, Dec. 2020, https://doi.org/10.1186/s13054-020-02859-w
-
D. Donnelly and M. L. Everard, “‘Dry’ and ‘wet’ cough: how reliable is parental reporting?,” BMJ Open Respiratory Research, Vol. 6, No. 1, p. e000375, Apr. 2019, https://doi.org/10.1136/bmjresp-2018-000375
-
L. Marcelino Sotelo Dias1 et al., “Physiotherapy practice for hospitalized patients with COVID-19,” Jornal Brasileiro de Pneumologia, p. e20220121, Aug. 2022, https://doi.org/10.36416/1806-3756/e20220121
-
A. Cakmak et al., “Physiotherapy and rehabilitation implementation in intensive care units: a survey study,” Turkish Thoracic Journal, Vol. 20, No. 2, pp. 114–119, Oct. 2019, https://doi.org/10.5152/turkthoracj.2018.18107
-
N. Ambrosino, N. Janah, and G. Vagheggini, “Physiotherapy in critically ill patients,” Revista Portuguesa de Pneumologia (English Edition), Vol. 17, No. 6, pp. 283–288, Nov. 2011, https://doi.org/10.1016/j.rppnen.2011.11.008
-
S. Younes, N. Ahmed, I. Ahmed, and E. Hassan, “Effect of multimodality chest physiotherapy interventions on prevention of ventilator associated pneumonia among mechanically ventilated patients,” Alexandria Scientific Nursing Journal, Vol. 24, No. 1, pp. 36–46, Mar. 2022, https://doi.org/10.21608/asalexu.2022.246005
-
B. Sañudo et al., “Potential application of whole body vibration exercise for improving the clinical conditions of COVID-19 infected individuals: a narrative review from the World Association of Vibration Exercise Experts (WAVex) Panel,” International Journal of Environmental Research and Public Health, Vol. 17, No. 10, p. 3650, May 2020, https://doi.org/10.3390/ijerph17103650
About this article
The authors would like to thank a French Company RespInnovation SAS, for their support by giving the opportunity to treat patients with “RespIn 11 Bronchial Airway Clearance System”. This is a High Frequency Chest Wall Oscillation device, which is very effective to release the lung airways of mucus and help patients expectorate. No sources of funding were used to assist in the preparation of this manuscript.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Laura Rutkauskienė: ideas; formulation or evolution of overarching research goals and aims. Conducting a research and investigation process, specifically performing the experiments, or data/evidence collection. Preparation, creation and/or presentation of the published work by those from the original research group, specifically critical review, commentary, or revision – including pre- or post-publication stages.
Goda Strautnikaitė: management activities to annotate (produce metadata), scrub data and maintain research data for initial use and later reuse. Preparation, creation and/or presentation of the published work, specifically visualization/data presentation.
Deividas Rutkauskas: application of statistical, mathematical, computational, or other formal techniques to analyze or synthesize study data.
Tomas Tamošuitis: management and coordination responsibility for the research activity planning and execution. Oversight and leadership responsibility for the research activity planning and execution, including mentorship external to the core team.
Raimondas Kubilius: preparation, creation and/or presentation of the published work by those from the original research group, specifically critical review, commentary, or revision – including pre- or post-publication stages.
Inesa Rimdeikienė: oversight and leadership responsibility for the research activity planning and execution, including mentorship external to the core team.
The authors declare that they have no conflict of interest.
The research met all applicable standards for the ethics of experimentation. All patients were instructed to sign a written informed consent after explanation about the details of the study procedures. Bioethics approved by Local Committee No. BEC-KN(B)-237.
