Abstract
This pilot study presents data on the application of two different physiotherapy techniques and the comparison of their effectiveness in patients with radiologically confirmed intervertebral disc herniation. At baseline and the end of the application of the studied physiotherapy techniques, the subjects, after being distributed into two groups, underwent testing in order to determine their trunk stabilizer muscle strength, pain intensity at rest and on exertion, and the level of disability. The physiotherapy program consisted of individually selected exercises. Subjects of the first group additionally underwent sling exercise therapy, and subjects of the second group – physiotherapy with feedback exercises. Both combinations – physiotherapy with feedback exercises and physiotherapy with sling exercise therapy – statistically significantly reduced functional disability and lower back pain at rest and on exertion. The physiotherapy program with feedback exercises was more efficient than the physiotherapy program with sling exercise therapy when correcting imbalance in trunk stabilizer muscle strength. The impact of both physiotherapy programs on trunk stabilizer muscle strength was similar. Both combinations – physiotherapy with feedback exercises and physiotherapy with sling exercise therapy – had an equal impact on the decrease in pain and functional disability
1. Introduction
Lumbar disc herniation is one of the most common causes of lumbar back pain and entails a significant social, psychological, and economic burden [1]. Chronic lower back pain (LBP) remains one of the major health issues worldwide [2,3]. During the last 14 years, the prevalence of LBP in the population increased from 3.9 % to 10.2 % [4].
According to the data of the Global Burden of Disease for the year 2010, LBP is among 10 diseases and traumas with the greatest burden in terms of the disability-adjusted life-years (DALY). In Great Britain, LBP was found to be one of the most common causes of disability among young adults, resulting in over 100 million work days lost per year [5]. Intervertebral disc herniation is one of the most common causes of lumbar back pain [1].
Numerous literature sources indicate that chronic LBP worsens the quality of life and is a costly health issue to the national economy. Most frequently, high costs are associated with prolonged treatment due to the insufficient efficiency of therapeutic techniques [3].
The issue of LBP has been widely analyzed in literature, yet no optimal treatment yielding the best results has been identified so far. LBP is treated pharmacologically and by applying various rehabilitation methods, including physiotherapy techniques.
Currently, a number of various physiotherapy techniques that have a positive effect on LBP patients are used in the world. One of the widely used techniques is the suspension system, which may help to identify muscles that are weak and fail to perform their function, and to strengthen such muscles [6]. Also, an alternative trainer system with feedback (Dr. Wolf) is gaining popularity.
The selection of the optimal treatment technique allows for achieving better results and saves money. When initiating LBP treatment, specialists should adequately evaluate the effectiveness of different physiotherapy techniques [3].
For this reason, timely application of appropriate rehabilitation techniques is highly important [7]. Even though LBP is a relevant problem worldwide, the effectiveness of its treatment via the application of physiotherapy techniques remains controversial. The analysis of scientific literature about the currently used techniques showed that none of these techniques proved to be clearly effective in the treatment of LBP. So far, there are no clearly defined protocols whose indications, classifying by the cause of pain, would warrant the application of a specific technique for maximum efficiency. In order to shorten the duration of rehabilitation, further and more extensive research is required, testing the efficiency of physiotherapy techniques and the respective rehabilitation protocols.
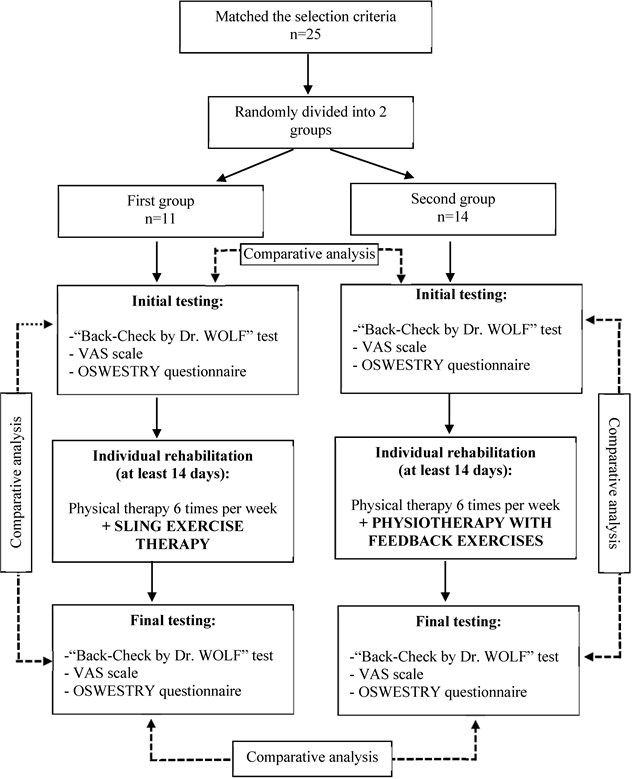
Fig. 1The scheme of investigation
2. Materials and methods
In this pilot study, we analyzed the effectiveness of sling exercise therapy and feedback exercises on trunk stabilizer muscle strength, pain, and functional disability in subjects with radiologically confirmed intervertebral disc herniation.
The study was performed with the permission of the Bioethics Committee, No. BEC-FMR(M)-282. The study included 25 patients – 15 females (60 %) and 10 males (40 %) – who met the following inclusion criteria:
• Radiologically confirmed intervertebral disc herniation in lumbar spine;
• Lower back pain with or without radiation to the leg;
• At least 2 weeks of inpatient treatment for LBP.
As this was a pilot study, we did not calculate the representative sample size, but rather included all subjects who met the inclusion criteria. The participants of the study were randomly distributed into two groups. The subjects’ mean age was 48.28 years. The patients indicated that the mean duration of pain was 16.76 (95 % CI 10.26-23.26) months. The duration of pain in the first group was 18.09 (95 % CI 10.12-26.02) months, and in the second group – 15.71 (95 % CI 4.97-26.46) months. The physiotherapy program consisted of individually selected exercises; subjects of the first group additionally underwent sling exercise therapy, and subjects of the second group - physical therapy with feedback exercises. Physiotherapy was applied six times weekly, the duration of each procedure being 40 minutes (Fig. 1).
2.1. Evaluation
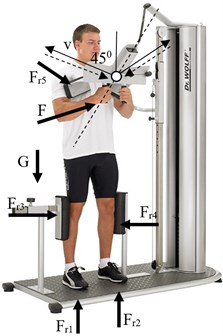
Muscle strength evaluation was carried out by using an electronic device Back-Check by Dr. Wolf, which with the help of two sensors measures the isometric strength (weight in kilograms) of the muscles of the back and the upper and lower limbs under the conditions of constant static resistance in a closed kinetic chain [8]. During the study, we evaluated isometric muscle strength during trunk flexion (Fig. 2), trunk extension (Fig. 3), trunk lateral flexion (Fig. 4), and hip extension (Fig. 5). Isometric muscle strength was evaluated by applying the same evaluation scheme in all subjects. All measurements of the same movement (flexion, extension, trunk lateral flexion and hip extension) were performed in triplicate, and the best result was included in the analysis. The duration of each movement was 10 seconds and muscle rest between the movements was 60 seconds. During the study, the diagnostic device evaluated the isometric muscle force as “very poor”, “poor”, “satisfactory”, “good”, or “ideal”, depending on the subjects’ characteristics (Figs. 6-8) [6].
Fig. 2Trunk flexion

Fig. 3Trunk extension

Fig. 4Trunk lateral flexion

Fig. 5Hip extension

Fig. 6The results of trunk extension and flexion evaluated with the Back-Check by Dr. Wolf equipment
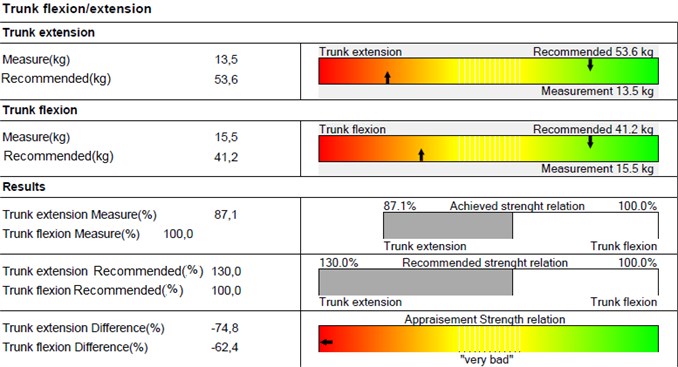
Fig. 7The results of trunk lateral flexion evaluated with the Back-Check by Dr. Wolf equipment
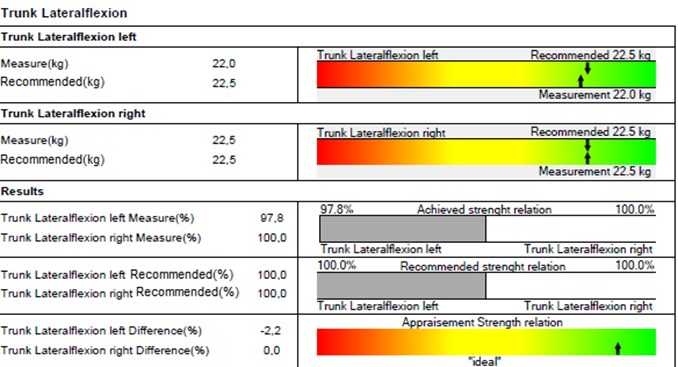
Fig. 8The results of hip extension evaluated with the Back-Check by Dr. Wolf equipment
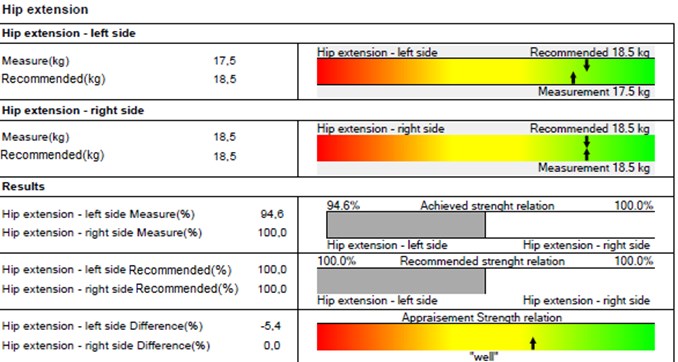
The characteristics of the evaluation obtained by using Back-Check by Dr. Wolf showed the balance of trunk flexion and extension (Fig. 6), trunk lateral flexion (Fig. 7), and hip extension (Fig. 8) in percent and kilograms. In addition to that, trunk flexion and extension (Fig. 6), trunk lateral flexion (Fig. 7) and hip extension (Fig. 8) were evaluated in a scale ranging from “very poor” to “ideal”, and the final evaluation was made (“very poor”, “poor”, “satisfactory”, “good”, or “ideal”).
Visual analog scale (VAS). The intensity of pain was evaluated by using a 10 cm visual analog numeric pain distress scale. This is a widely used tool for pain evaluation [9]. In this scale, “0” refers to the absence of pain, and “10” – to unbearable pain. This scale has been proven to have sufficient suitability, validity, and reliability in testing patients with lower back pain [10].
Oswestry questionnaire. The Oswestry questionnaire was used to evaluate to which extent pain influenced the areas of activity listed in 10 sections of the questionnaire. This is the oldest and best researched questionnaire for the evaluation of functional status and disability. It was developed specifically for the evaluation of LBP. Its biggest shortcoming is that it primarily focuses on patients’ daily physical activity, paying very little attention to psychosocial problems [11].
Calculation of the Oswestry Disability Index (ODI). Each of the response letters were evaluated in points from 0 to 5: A – 0, B – 1, C – 2, D – 3, E – 4, and F – 5. The points were then added up, the maximal sum score (50 points) meaning severe dysfunction and the minimal score (0 points) – good evaluation of the function. The percentage of the score was calculated by applying the following formula:
Sum score / 50 x 100 = percentage (%)
The percentage of the score ranged from 0 to 100 %, lower percentage meaning lesser influence of lumbar back pain on the patient’s functional status, and vice versa. Conclusions were made on the basis of the following percentage distribution of the score:
0-20 % – minimal disability;
21-40 % – moderate disability;
41-60 % – severe disability;
61-80 % – crippled;
81-100 % – bed-bound/exaggerating the symptoms.
2.2. Physiotherapy program applied in the first studied group
The physiotherapy program assigned to the patients of the first group consisted of conventional exercises performed in various positions – i.e. when the patient is lying supine, on the side, lying prone, and in the quadruped position. During this program, the emphasis was placed on postural muscle-strengthening exercises and stretching exercises. As an additional physiotherapy program, sling exercise therapy (with Redcord equipment) was applied in this group of patients. When applying the sling exercise therapy, the whole body or a certain body part was suspended on the ropes, thus creating the condition of controlled instability and removing the effect of gravity. Active and passive movements were performed in the vertical, horizontal, and sagittal planes. At first, lower-intensity isometric exercises for the target muscles were performed, subsequently gradually involving all other agonist muscles, thus simultaneously strengthening the stabilizing and the dynamic functions. The selection and the dosage of the exercises were adjusted by taking into account the weak body areas and body imbalance. A single session of the program lasted 40 minutes; each session was repeated 6 times per week. Exercise with Redcord equipment performance examples are illustrated in Table 1.
Table 1Exercises with Redcord equipment.
Exercises with Redcord equipment | Description of exercises |
 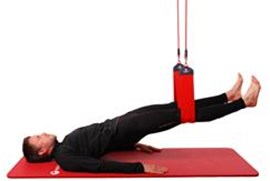 | Supine Pelvic Lift focus on functional stability and neuromuscular control in the lower back, abdominals and pelvis and hip musculature. This is one of the most commonly used exercises with Redcord. Required equipment: Redcord Trainer or Redcord Mini, two narrow slings or two straps. Starting position: Lie on your back with arms parallel to body. The height of the narrow slings/straps should be so that knees are bent 90 degrees with feet on surface. Instructions: Straighten knees and lift your pelvis from surface in a slowly and controlled movement. Lift until body is straight (see picture). Emphasize that left and right side of your pelvis is at the same height. Hold the position for 2-3 seconds before returning to starting position in a controlled movement. Perform 5 repetition of 3 sets. |
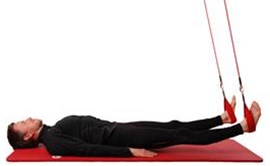  | Supine Knee Flexion focus on the hip and knee region and especially the hamstrings. At the same time the exercise challenges core control. Required equipment: Redcord Trainer or Redcord Mini, two straps. Starting position: Lie on your back with arms parallel to body and suspension point above hips. Place straps at heels. The height of the straps should be about 20 cm above surface. Instructions: 1. Lift pelvis up to a straight body position in a slowly and controlled movement. 2. Then press heels into straps and pull heels towards buttocks. Emphasize that left and right side of the pelvis is at the same height throughout the movement. Return to starting position. Perform 5 repetitions of 3 sets. |
2.3. Physiotherapy program applied in the second studied group
The physiotherapy program assigned to the patients of the second group consisted of conventional exercises performed in various positions – i.e. when the patient is lying supine, on one side, then on the other side, lying prone, and in the quadruped position. During this program, the emphasis was placed on postural muscle-strengthening exercises and stretching exercises. As an additional physiotherapy program, exercise training with five Back-Check by Dr. Wolf trainers with feedback, designed for strengthening trunk stabilizer muscles, was applied in this group of patients.
An increase in the activity of segment stabilizer muscles may not be achieved via conventional dorsal muscle-strengthening training. Conventional trainers for dorsal muscles activate the large muscles of the back, when the person sitting in the trainer makes the muscles work by maintaining a certain position. Here lies the essential difference between conventional and Dr. Wolf trainers and the movement technique. During the exercise with Dr. Wolf trainers, deep segmental spinal stabilizer muscles are activated. Small ranges of motion and coordination-requiring exercises ensure the stimulation of the transverse abdominal muscles (m. transversus abdominis) and the lumbar multifidus muscle (m. multifidus lumbalis). Dorsal muscle strengthening is performed in three planes – the sagittal, the frontal, and the transverse ones. Besides, the exercises are performed in three different positions – sitting, lying, and standing.
Feedback. Dr. Wolf trainers are equipped with feedback tools that may perform visual evaluation of the movement and the body posture during the exercise. Digital sensors register even the slightest movement and present the obtained data in the optical display, thus providing feedback on muscle contraction/activity.
Dr. Wolf back therapy system consists of 5 different trainers.
2.3.1. Trainer I
The exercise activates and strengthens the lumbar multifidus muscle (m. multifidus lumbalis) and increases the mobility of the lower back. The exercise is performed in the sitting position (with feedback), (Fig. 9).
Fig. 9Trainer I

Fig. 10Trainer II
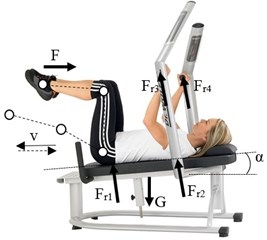
Fig. 11Trainer III

Fig. 12Trainer IV

Fig. 13Trainer V
2.3.2. Trainer II
The exercise activates and strengthens the transverse abdominal muscles (m. transversus abdominis) and increases the mobility of the waist and the pelvis. The exercise is performed in the lying position (with feedback), (Fig. 10).
2.3.3. Trainer III
A daily standing position, where, with the help of a sensor, the patient learns to activate trunk stabilizer muscles in the standing position (with feedback), (Fig. 11).
2.3.4. Trainer IV
The exercise provides activation of back stabilizer muscles in the standing position with force directed to the shoulder and the contralateral hip, thus training the patient to stabilize the lateral muscles of the trunk in the standing position (with feedback), (Fig. 12).
2.3.5. Trainer V
The exercise provides unique activation of the stabilizer muscles of the back in the vertical position with the pelvis fixed. The controlled range, speed, and angle of the movement allow for an objective evaluation of the activity of the stabilizer muscles with feedback, (Fig. 13).
2.4. Statistical data analysis
Statistical data analysis was performed using statistical software Microsoft Office Excel 2010 and IBM SPSS Statistics 22. Quantitative data are presented as arithmetic means (m) and confidence intervals – m (95 % CI). Qualitative data are presented as percentage. Two dependent samples were compared by applying the non-parametric Wilcoxon test. Differences of < 0.05 were considered to be statistically significant.
3. Results
Chronic lower back pain (LBP) remains one of the major health issues worldwide [3]. Studies have shown that between 60 % and 90 % of the population sustain lower back injuries at least once during different periods of their lives, and from 15 % to 42 % of such people suffer from back pain as a result [2]. During the last 14 years, the prevalence of LBP in the population increased from 3.9 % to 10.2 % [4].
During our study, pain intensity was evaluated at rest and on exertion. In the first group of the subjects (sling exercise therapy), the mean pain intensity score at rest before the physiotherapy program was 4.27 (95 % CI 2.99-5.55), and in the second group (physiotherapy with feedback exercises) – 3.93 (95 % CI 2.93-4.93). After the physiotherapy programs, pain intensity at rest dropped both in the first and the second groups of subjects – respectively, to 2.64 (95 % CI 1.42-3.85) and 2.07 (95 % CI 1.15-2.99).
The study showed that physiotherapy techniques applied in both subject groups statistically significantly reduced LBP (in the first group, = 0.007, = –2.699; and in the second group, = 0.002, = –3.093). The effectiveness of physiotherapy when applying sling exercise therapy in LBP reduction has also been noticed by other authors. Kline et al. (2013) stated that the application of this technique during physiotherapy sessions reduced PBP and disability in ballet dancers [12].
The evaluation of the balance of trunk stabilizer muscle strength before physiotherapy with sling exercise therapy and physiotherapy with feedback exercises showed that in the first group of subjects, the balance deviation was 49.04 (95 % CI 32.10-65.98) from 0, and in the second group – 60.39 (95 % CI 40.05-80.73) from 0 (Fig. 14).
Fig. 14The difference in the subjects’ back and abdominal muscle strength ratios before and after rehabilitation. * – p < 0.05 non-parametric Wilcoxon test comparing distributions (before and after rehabilitation)
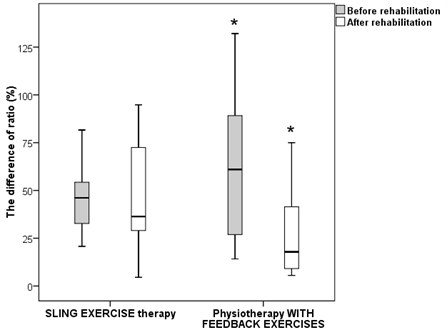
After the application of physiotherapy programs, the balance deviation changed – in the first group of subjects, it was 48 (95 % CI 27.44-68.59) from 0, and in the second group – 28.1 (95 % CI 14.03-42.14). In the first group, the change in the balance was not statistically significant ( = 0.79, = –0.267), whereas in the second group, the change in the balance of the muscle strength following physiotherapy was statistically significant ( = 0.006, = –2.731), indicating a significant shift of the back and abdominal muscle strength ratio towards the recommended balance.
In the first group of subjects, the evaluation of the balance of the lateral muscles of the waist prior to the application of the physiotherapy program revealed a muscle strength imbalance reaching 19.87 % (95 % CI 10.29-29.46). In the second group, this imbalance reached 16.22 % (95 % CI 9.15-23.29) (Fig. 15).
Fig. 15The balance of the subjects’ trunk lateral flexion on the left and the right sides before and after rehabilitation. * – p < 0.05 non-parametric Wilcoxon test comparing distributions (before and after rehabilitation)
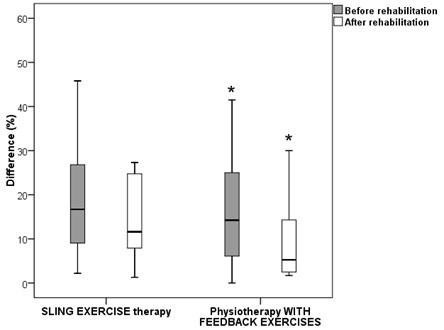
After the application of the physiotherapy program, the balance of the lateral muscles of the waist changed and, on the average, reached 20.31 % (95 % CI 7.15-33.46) in the first group of subjects, and 10.28 % (95 % CI 3.95-16.60) – in the second group. In the first group, no statistically significant change was observed in the balance of the lateral muscles of the waist ( = 0.894, = –0.133). In the second group, the change was statistically significant ( = 0.03, = –2.166), which indicates a shift in the balance of the muscle strength towards the recommended equilibrium (Fig. 15).
According to the results of the Oswestry questionnaire, the mean evaluation of disability in the first group of subjects prior to physiotherapy was 20.36 points (95 % CI 16.20-24.53), and in the second group – 17.43 points (95 % CI 13.88-20.98) (Fig. 16).
Fig. 16The Oswestry Disability Index in the subject groups before and after rehabilitation. *,** – p < 0.05 non-parametric Wilcoxon test comparing distributions in groups (before and after rehabilitation)
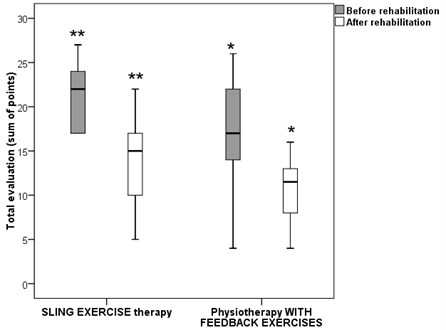
After the application of the physiotherapy program, the mean evaluation of disability in the first and the second groups of subjects was, respectively, 13.36 (95 % CI 9.72-17.01) and 10.43 (95 % CI 8.37-12.49) points. The change in the evaluation of disability was statistically significant in both groups (in the first group, = 0.005, = –2.814, and in the second group, = 0.002, = –3.063) (Fig. 16).
4. Discussion
It has been widely accepted that the main causes of LBP are poor posture and the imbalance of the isometric force of core muscles [13]. Our study involving the application of physiotherapy with sling exercise therapy and physiotherapy with feedback exercises showed a statistically significant improvement of trunk stabilizer muscle strength balance after physiotherapy with feedback exercises. In case of physiotherapy with sling exercise therapy, other authors have also noticed this trend [14]. Sling exercise therapy improved the balance of trunk stabilizer muscles and significantly reduced LBP [14]. A systematic analysis conducted by Lee (2014) showed that sling exercise therapy with additional application of individualized physiotherapy allows for expecting a more favorable increase in trunk stabilizer muscle strength and a decrease in LBP [14].
Prior to selecting the physiotherapy program for LBP patients, the evaluation of the symmetry of dorsal and abdominal muscle strength is highly important for setting an appropriate intensity of physical exercise, as imbalance of the core muscle strength may be one of the causes of LBP [16]. We did not find any literature data on the effect of these two physiotherapy programs on the balance of trunk stabilizer muscles. Our study on the balance of the trunk stabilizer muscle strength when applying physiotherapy with sling exercise therapy and physiotherapy with feedback exercises showed that physiotherapy with feedback exercises was more effective in reducing muscle strength imbalance, as the muscle strength balance after the application of this program was closer to the recommended norms. We could not evaluate the effect balance improvement on pain and disability reduction as there was no difference in these findings between the groups before and after the application of physiotherapy programs. We think that the effect of sling exercise therapy on the restoration of the balance of muscle strength is disputable, as we frequently observed overtraining of trunk stabilizer muscles without any change in muscle strength balance – and sometimes this balance even deviated further away from the recommended norm.
5. Conclusions
The comparison of our results with those obtained by other authors revealed a lack of publications on the application of physiotherapy with sling exercise therapy and physiotherapy with feedback exercises for LBP reduction. When evaluating trunk stabilizer muscle strength, we used Dr. Wolf Back-Check equipment, which evaluated the strength in kilograms. Literature data on the effect of trunk stabilizer muscle strength on balance and LBP reduction are scarce, and mostly focus on muscle endurance. Our study showed that both physiotherapy with sling exercise therapy and physiotherapy with feedback exercises statistically significantly reduced functional disability, and relieved lower back pain at rest and on exertion. However, physiotherapy with feedback exercises was more effective in restoring the balance of the trunk stabilizer muscle strength. In general, it should be emphasized that further studies are required on this topic, as the small number of studies on the efficiency of this physiotherapy program prevents us from comparing our results with those obtained by other authors.
References
-
Devon I. R. Epidemiology and risk factors for spine pain. Neurologic Clinics, Vol. 25, Issue 2, 2007, p. 353-371.
-
Illés T. S., Schiopu D., Ouahes R., Penders W., Reynders P. F. Therapeutic algorithm for low back pain. Medical Journal of Brussels, Vol. 36, Issue 4, 2015, p. 307-312.
-
Macedo L. G., Latimer J., Maher C. G., Hodges P. W., Nicholas M., Tonkin L., et al. Motor control or graded activity exercises for chronic low back pain? A randomised controlled trial. BioMed Central Musculoskeletal Disorders, Vol. 9, Issue 65, 2008.
-
Freburger J. K., Holmes G. M., Agans R. P., Jackman A. M., Darter J. D., Wallace A. S., et al. The rising prevalence of chronic low back pain. Archives of Internal Medicine, Vol. 169, Issue 3, 2009, p. 251-258.
-
Duthey B. Background Paper 6.24 Low Back Pain. http://www.who.int/medicines/areas/ priority_medicines/BP6_24LBP.pdf, 2013.
-
Mockevičienė D., Bakanovienė T., Savenkovienė A., Vaitkevičius J. V., Miliūnienė L. Assessment of the isometric muscle force balance in persons having back pains. Health Sciences, Vol. 22, Issues 5-84, 2012, p. 9-12.
-
Chou R., Huffman L. H. American Pain Society, American College of Physicians. Nonpharmacologic therapies for acute and chronic low back pain: a review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline. Annals of Internal Medicine, Vol. 147, Issue 7, 2007, p. 492-504.
-
Savenkovienė A., Mockevičienė D. Impact of visual impairment on balance of isometric strength of separate muscular groups of adults. Young Scientists Research, Vol. 4, Issue 33, 2011, p. 174-180.
-
Caren F., Ozcan A. The relationship of the Functional Rating Index with disability, pain, and quality of life in patients with low back pain. Medical Science Monitor, Vol. 12, Issue 10, 2006, p. 435-439.
-
Smeets R. J., Van Geel A. C., Kester A. D., Knottnerus J. A. Physical capacity tasks in chronic low back pain: what is the contributing role of cardiovascular capacity, pain and psychological factors? Disability and Rehabilitation, Vol. 29, Issue 7, 2007, p. 577-586.
-
Gatchel R. J., Mayer T. G., Theodore B. R. The pain disability questionnaire: relationship to one-year functional and psychosocial rehabilitation outcomes. Journal of Occupational Rehabilitation, Vol. 16, Issue 1, 2006, p. 75-94.
-
Kline J. B., Krauss J. R., Maher S. F., Qu X. Core strength training using a combination of home exercises and a dynamic sling system for the management of low back pain in pre-professional ballet dancers: a case series. Journal of Dance Medicine and Science, Vol. 17, Issue 1, 2013, p. 24-33.
-
Janulis M., Samėnienė J. The rehabilitative effects of the spine stabilization and posture correction exercise course on trunk muscle isometric strength and its symmetry in patients with lumbar disc herniation. Complementary and Alternative Medicine in Science, Vol. 1, Issue 2, 2013, p. 29-33.
-
Kim J. H., Kim Y. E., Bae S. H., Kim K. Y. The effect of the neurac sling exercise on postural balance adjustment and muscular response patterns in chronic low back pain patients. Journal of Physical Therapy Science, Vol. 25, Issue 8, 2013, p. 1015-1019.
-
Lee J., Yang S., Koog Y., Jun H., Kim S., Kim K. Effectiveness of sling exercise for chronic low back pain: a systematic review. Journal of Physical Therapy Science, Vol. 28, Issue 8, 2014, p. 1301-1306.
-
Lee J., Hoshino Y., Nakamura K., Kariya Y., Saita K., Ito K. Trunk muscle weakness as a risk factor for low back pain: a 5‐year prospective study. Spine, Vol. 24, Issue 1, 1999, p. 54-57.
About this article
Eglė Lendraitienė – preparation of research design and methodology, data interpretation and discussion, drafting and revising the article. Kazimieras Poškys – acquisition of data, physiotherapy program application, drafting and revising the article. Daiva Petruševičienė – article introduction, discussion, drafting and revising the article. Kristina Berškienė – analysis and interpretation of data, drafting and revising the article. Vilma Mauricienė – analysis and interpretation of data, drafting and revising the article.
